Plum Health Blog
Direct Primary Care Conference 2017
Today I'm blogging from Orlando! The 2017 Direct Primary Care Nuts and Bolts 2.0 conference is ongoing! There are some heavy hitters in the room, and it's great to meet up with colleagues and learn best practices. Moreover, this is a call to action - it's inspiring being surrounded by 250 of the leaders in the Direct Primary Care movement!
These doctors have left a secure paycheck, given up on their employed gigs and pursued their dream of delivering the best care possible for their patients. I'm always inspired by their courage in the face of uncertainty and their dedication to lifting up the profession of primary care.
One of the most inspiring talks of this conference was given by Dr. Doug Farrago. He received a standing ovation after sharing his truth about why he's a Direct Primary Care doctor. He detailed his trajectory from being a battered employed doctor, threatened with termination if he questioned his marching orders, to leaving the system and practicing in a DPC model with fulfillment.
A big thanks to Dr. Lee Gross and the Docs 4 Patient Care team who have organized this conference. I'm looking forward to 'next time'!
- Dr. Paul with Plum Health in Detroit, Michigan
Mentoring Students at Wayne State University School of Medicine
Part of my mission, part of the "why" behind what I do, is to educate medical students and inspire them to choose a career in primary care specialties. Primary care doctors have the greatest impact on their communities, have the most tools at their disposal, and are most able to bend the cost curve in the health care ecosystem.
As a part of that mission, I spend a good amount of time interacting with medical students at Wayne State University School of Medicine (WSUSOM). This week, I took part in two different events at WSUSOM. The first was a mentoring session for first year students and the second was a mock interview session for the fourth year students.
For the first year students, it's an opportunity to get to know each other, learn from each other, and to be a resource. For the fourth year students, it's an opportunity to help them polish their interviewing skills as they prepare for the next step in their careers - residency!
This next generation of doctors will face significant changes and challenges in the health care system - from greater automation, to precision medicine, to even Artificial Intelligence. I hope that I can be a part of the foundation along with their formal education at WSUSOM that sets them on the right path to success in medicine.
Thanks for reading, and have a beautiful day,
- Dr. Paul Thomas with Plum Health DPC
Volunteer Doctor at Tour de Troit 2017
One of my favorite events in Detroit is the Tour de Troit, a friendly 25 mile bike ride through Detroit and some of its beautiful neighborhoods. For the last 5 years, I've been participating as a volunteer medic, starting during my medical school training and continuing through residency, and now as a doctor.
I love the ride because I get to see so many people who I know! There are so many people and businesses that support this ride and who make it a really special event. From the Great Lakes Coffee that's served with food from the Detroit Institute of Bagels, to the lunch after the ride from local restaurants, to all of the people from the community who come out and either volunteer or ride. It all adds up to a great time.
Biking is also a super healthy way to see the city, and during the ride we have police barricades and police escorts, so it makes for a very safe environment for everyone who participates. A big thank you to the Detroit Police Department for keeping everyone safe again this year!
When I talk about health, I'm not only talking about physiological health, but also social health - I believe that events that bring together people from different communities and backgrounds can serve to strengthen our region and make us better. That's why I love Tour de Troit, because it is this space where people from across Metro Detroit come together. For future events in this same vein, check out Slow Roll or Open Streets Detroit.
It's always a great ride, but it comes with a few injuries every year. This year the head count was about 7,000 riders and we had a handful of accidents and injuries to attend to throughout the day. There were about 20 of us medical volunteers, mostly medical students, and we delivered basic first aid for riders after minor injuries. For more major events, Emergency Medical Services were used.
So, with fall and cooler weather fast approaching, make it a point to get out today, tomorrow, and the next day on a bike ride or a walk or a run - this is a great time to be active and healthy, and your body, mind, and spirit will thank you for the effort.
Thanks for reading, and have a great day!
- Dr. Paul with Plum Health
Wayne State White Coat Ceremony Speech
The White Coat Ceremony, a New Tradition
The annual White Coat Ceremony is a relatively new tradition at medical schools across the country. In order to convey the virtues of the profession - compassion, altruism, duty, honor, respect, and responsibility - Dr. Arnold P. Gold created the event.
The first White Coat Ceremony was held at the Columbia University College of Physicians and Surgeons in New York in 1993. Dr. Gold believed that students should declare their commitment to the profession and the virtues therein at the beginning of their medical school journey, rather than at the end.
Now, 97% of medical schools have a White Coat Ceremony. The Ceremony gives a clear set of guidelines for these doctors-in-training to follow, and students are able to accept the obligations of the profession and commit to upholding the high standards that come with the title of "doctor".
The Declaration of Commitment
I solemnly pledge myself to consecrate my life to the service of humanity;
I will give to my teachers the respect and gratitude which is their due;
I will develop my skills with conscience and dignity;
The health of my patients and myself will be my first considerations;
I will respect those things that are confided in me;
I will maintain by all the means in my power the honour and the noble traditions of the medical profession;
My colleagues will be my comrades;
I will not permit considerations of religion, nationality, race, party politics, sexual orientation, or social standings to intervene between my duty, my peers, and my patients;
I will maintain the utmost respect for human life and I will not use my medical knowledge contrary to law;
I make these promises solemnly, freely and upon my honour.
My Speech
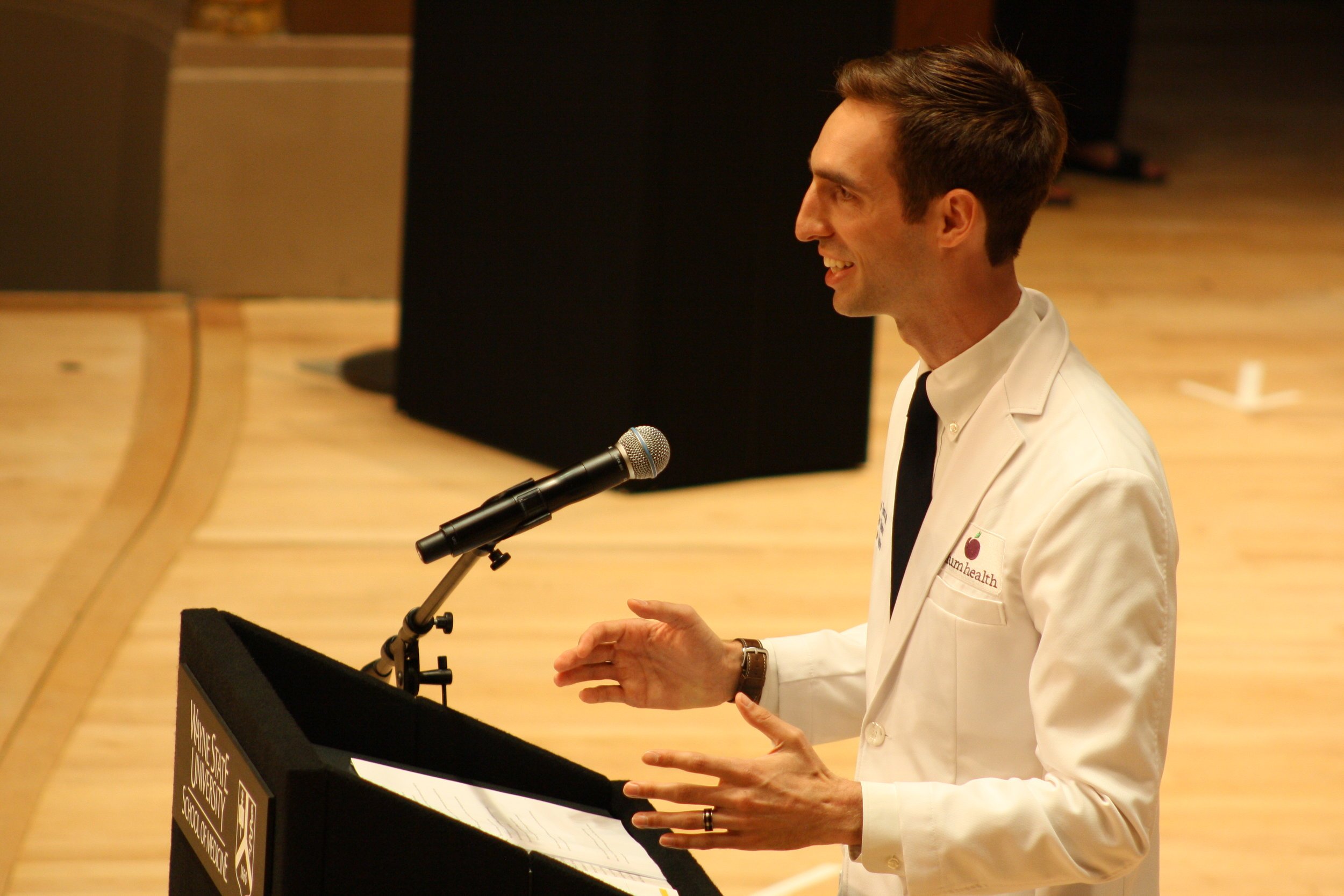
First of all, it was a tremendous honor to be selected as the Keynote Speaker for the Wayne State University School of Medicine White Coat Ceremony for the Class of 2021. When I received the phone call to be the speaker, I was nearly speechless and unsure of my ability to live up to the expectations that come with this role. I needed 24 hours to think on the offer.
After talking it over with my wife, I decided that this was something that I could do, and that I had a lot to say about the opportunity before these students and the medical profession in general.
When I was getting ready for medical school, I read several books. I was to be the first doctor in my family and I had a limited perspective on the medical field, i.e. I had no idea what I was getting myself into.
One of the authors that stuck with me was Atul Gawande, a surgeon and writer out of Boston. He wrote about the appealing aspects of a career in Medicine: autonomy, complexity, and a direct relationship between effort and reward.
However, something was missing. For me, that something is happiness. You see, doctors struggle with professional burnout, substance abuse, and suicide. We can speculate about why, but I think it's some combination of consistent perfection, frustrations with the monolithic systems within health care, and a heavy workload. I didn't want to get into the darker side of these concerns during the White Coat Ceremony, but they definitely influenced my speech.
Because of these concerns and these problems in the medical profession, I believe that we need to focus on creating a culture of happiness in the medical field. How can we train doctors to be happy? How can we create hospital systems, clinics, and insurance policies that foster physician wellness and happiness?
I don't know if there are great answers to these questions, but it's something that I have thought about deeply. For me, creating a happy practice involved creating a membership model for health care via Plum Health. That works for me, but during my speech, I encouraged these medical students to explore the profession fully and to find their own means of happiness within it.
I wish the very best to the WSU SOM Class of 2021. I know that these students will be a part of a generation of doctors that revolutionizes the way we deliver high-quality, compassionate health care. Without further ado, my speech:
Thanks for reading and for watching, and have a wonderful day,
- Paul Thomas, MD | Doctor with Plum Health in Detroit, Michigan
Wayne State University School of Medicine published an official write-up about the event on their webpage, here.
Street Medicine Detroit
This month I had the opportunity to volunteer with Street Medicine Detroit, an organization dedicated to helping homeless people in Detroit with their medical care. This was an organization that I volunteered with and supported during its early days at Wayne State University School of Medicine.
The service is run by WSU medical student volunteers and they go out to different locations across Detroit and assist those who need medical care. This can be done on street corners, in soup kitchens, homeless shelters, and churches across the city.
This month, I met up with the volunteering students at Manna Community Meal to deliver health care services. This is in the basement of St. Peter's Episcopal Church in Detroit's Corktown neighborhood. It was a great way to give back, and if you want to support Street Medicine, they take donations at their website, here.
Talking with a group of medical students while volunteering with Street Medicine Detroit at St. Peter's Episcopal Church in the Corktown Neighborhood of Detroit, Michigan.
Plum Health Advocating for Direct Primary Care in Washington DC
This week we're in Washington DC, advocating for affordable, accessible healthcare services on Capitol Hill. We're meeting with the offices of Senator Stabenow, Senator Peters, Congresswoman Lawrence, and Congressman Conyers. This is one of those moments where I feel like the mission that I'm on is bigger than the community that I live in and bigger than my city and my state. Access to affordable health care is a National concern and our representatives and their office personnel have given us open ears.
On Thursday morning, I boarded a plane to DC. That day, I met up with several of my Direct Primary Care colleagues at the DPC Summit 2017. We took a bus from our hotel in Crystal City to the Dirksen Building on Capitol Hill. We received instructions from our advisors about how to talk to our legislators: be authentic and tell your story.
Here's the video I shot in the Detroit Metro Airport prior to taking off:
After our briefing, I was able to meet up with legislative assistants from the offices of Senator Stabenow, Senator Peters, Congressman Conyers, and Congresswoman Lawrence. Here's a video I shot inside the atrium of the Hart Senate Office Building:
The Hart Senate Office Building houses the offices of Senator Peters and Senator Stabenow. I was bouncing between this building and the Rayburn House Office Building, where Congresswoman Lawrence and Congressman Conyers have their offices. Here's a video I shot just outside of the Rayburn House Office Building:
Thanks for reading and watching, and have a great day,
- Dr. Paul Thomas with Plum Health DPC in Detroit, Michigan
Primary Care Clinic in Detroit
When I was a first year medical student, I worked with a group of my fellow medical students to build an outdoor medical clinic. We wanted to raise awareness about the lack of primary care services in Detroit, and we accomplished this by constructing an outdoor medical clinic.
Currently, there are roughly 50 - 100 primary care doctors in the City of Detroit. This equates to about 1 primary care doctor for every 6,000 - 12,000 residents, which is horribly underserved. In the future, I would like to see 1 primary care doctor in every single Detroit Neighborhood, from East English Village to Ford/Wyoming, from Old Redford to Lafayette Park.
Having community primary care doctors creates a tremendous amount of value for the surrounding neighborhood - that doctor becomes a go-to person for folks who need health care and even emotional support.
However, the current reality in Detroit is that folks either don't have access to a primary care doctor or are driving to the suburbs for their care. To illustrate that lack of primary care services, our group of medical students built an outdoor clinic as a part of the Heidelberg Project on Detroit's East Side or what you may call the McDougall Hunt Neighborhood. Of course, we had the approval of Tyree Guyton, who checked in on our work that day, and we also received some press from the Detroit Free Press and the Wooster Collective out of NYC.
It was a simple clinic, with a reception desk, a door frame, a door, an exam table, and some chairs. On the door, we wrote all of the barriers to accessing health care services in Detroit and in the Nation. This was in 2009, when the debate over the Affordable Care Act was raging.
I visit the location periodically, to see how it has changed over the years. The last time I visited the site was in September 2016 during the Tour de Troit, an annual bicycling event that takes riders around the city. Someone had added a skeleton and some body parts, and it looks like Tyree made his signature drawings of faces on our plexiglass wall.
Plum Health may be in its infancy, but I know that we are already filling a need in the community in terms of primary care services. We recently surpassed 100 members and continue to grow, adding new members each week. We've taken care of newborns, toddlers, teens, and adults, and have addressed conditions ranging from sore throats to cancer.
As I continue to serve in the community, I hope to live up to the ideals that I put forth in this work of public art, to be the kind of community doctor that addresses the lack of access to health care in Detroit. I will also work to inspire the next generation of Family Physicians to take the leap into private practice in a community-based setting.
Thanks for reading, and have a wonderful day,
Dr. Paul Thomas with Plum Health DPC
How to Quit Smoking in Detroit
The adult smoking rate in Michigan is 20.5%. So, of the Michiganders over the age of 18, roughly 1 in 5 are smokers and that translates to 1,557,000 smokers in the State of Michigan. Among the United States, Michigan has the 9th highest smoking rate among adults.
This is unfortunate because there are many adverse effects of smoking, from increasing the risk of heart attacks and strokes to increases in the rates of head and neck cancers and lung cancers.
However, there are effective treatments that can help you quit smoking, and once you quit smoking many health benefits can be realized, from lowering your blood pressure to decreasing your risks of cancer.
This week, I've had a few people ask for help in terms of smoking cessation, and I am happy to provide that type of help. In fact helping people to quit smoking has some of the best patient-oriented evidence in medicine. Full stop.
Logistically, I would have you come in for an appointment. We would talk about where you are - pre-contemplation, contemplation, or ready to quit aka "quit mode". Then we'd review your medical history, current medications and any pertinent health-related issues. We would then formulate a treatment plan based on you as an individual.
In the person discussed in this video, we used Zyban or Wellbutrin or Bupropion (all different names for the same medication). This is effective in reducing the cravings that people feel for cigarettes. Then, we set a quit date. This is 1 week after starting the Zyban (bupropion).
After the quit date is reached, nicotine replacement therapy is used to tamp down hour-to-hour cravings. This can be in the form of a patch or gum or lozenges. Again, we personalize the method based on your preferences.
Let me know if you'd like to start your journey to better health with Plum Health, you know that you can reach me through our contact page or by phone, 313.444.5630.
Sincerely,
Dr. Paul Thomas with Plum Health DPC
WeWork Creator Awards Detroit Application
Today, we submitted our application for the WeWork Creator Awards! I really enjoy submitting applications for contests like this, because it helps me to clarify our mission, vision and values. And it's an opportunity to learn and grow through outside feedback about our internal operations.
In the application, they ask: "What problem is your idea, business, or organization solving?" For us at Plum Health, it's all about providing high-quality Family Medicine services in the community. It ain't sexy and it ain't super exciting, but it's so darn necessary! Having excelling primary care services in your neighborhood saves costs and improves health outcomes.
As they put it in this linked article, "One primary care doctor per 10,000 people in the U.S. can decrease hospital admissions by 5.5 percent, emergency room visits by 11 percent and surgeries by 7 percent."
This point is salient in Detroit, where there is an epic primary care shortage. Currently, there are only 50 - 100 primary care doctors in the City of Detroit for 680,000 people. That's 1 doctor for every 6,000 - 12,000 people. I recently wrote an article about this in the Detroit News.
Historically, this has been a difficult issue to solve because practice location for doctors is often tied to reimbursement from the community. Primary care doctors have avoided Detroit because more than half of Detroiters are on Medicaid, which generates low reimbursements.
With Plum Health, we do not rely on government or third party payers of reimbursement. Instead, we bill patients directly: $10/month for children and $49 for young adults, which covers all doctor's visits, texts, phone calls, and emails.
Additionally, members also have access to wholesale medications, at-cost lab work, and at-cost imaging services. From January - May 2017, we have saved our members roughly $15,000 on their meds, labs, and imaging. We are here to provide a tremendous amount of value to our patients and our community.
Our ask for the WeWork Creator Awards: help us reach our goal of providing value for the community by supporting what we do at Plum Health DPC!
The WeWork application continued with the following question: "How do you, your business, or your organization interact with the community?" Put simply - we are imbedded within the community and provide ours services to community members.
At Plum Health DPC, we take care of folks of all ages, races, ethnicities, and orientations. We are practicing on the street level, open and accessible to the community. Our youngest member is 14 months old, our oldest is 63 years; some of our members earn less than $30,000 and cannot otherwise afford health care. These folks are often shut out of the traditional insurance system because they cannot afford the premiums.
In addition to serving our paying customers in the community, I regularly volunteers at Cass Community Social Services' Clinic in Cass Corridor and the Student Run Free Clinic at I-94 and Conner. Here, I'm able to deliver free care to the most vulnerable members of the community - typically the homeless and uninsured.
Finally, Plum Health is regularly at health fairs throughout Detroit, performing free health screenings for non-profit organizations and church groups.
The last major questioned asked in the application was about how we would use the money if we won: "If you were awarded a grant, what new benchmarks would you be able to reach?" We are doing pretty well at Plum Health, adding new members each month and growing at a sustainable pace. However, if we won the Creator Award, we would be able to grow more quickly and therefore serve more people in Detroit and beyond.
Specifically, A grant of $18,000 - $36,000 would allow us to lease a larger office space and hire a second doctor. In a city with such limited primary care options, hiring a second doctor to work in the city would make a substantial difference in the lives of the people in our community.
We've taken care of folks who earn less than $30,000 and we've seen people who haven't been to a doctor in years, living in fear of generating large medical bills, and living with the consequences of their worsening high blood pressure and diabetes. Without the grant, the goal of leasing a larger office space and hiring a doctor would be at 6 - 12 months. With the grant, these goals would be achieved in 3 - 6 months.
Thanks so much for reading more about what we do at Plum Health DPC, and if you're a member of the WeWork community, thanks for taking the time to read our application and this blog post!
Sincerely,
- Dr. Paul with Plum Health DPC.
Direct Primary Care in St. Clair Shores
Last month, we were invited to a Health Care Forum in St. Clair Shores, Michigan with Senator Patrick Colbeck. We had a great meeting, with about 30 - 40 members of the community who are interested in the principles of free market healthcare that we discussed.
Senator Colbeck has been making a tour across the State of Michigan, talking with folks in similar forum-type settings about health care and ways that we can reform our primary care system. The last Town Hall that I was able to attend was in Grosse Pointe. The aim is to deliver higher-quality care with better service and at a lower price. Senator Colbeck is a staunch supporter of Direct Primary Care services and he has proposed a Medicaid Pilot program at the State level for DPC services.
Here's the portion of the talk that featured Plum Health DPC and the services that we provide:
Senator Colbeck spoke about the legislative efforts to advance Direct Primary Care at the State Level in his speaking slot, and to conclude the evening, we took time to answer questions from the audience about DPC, insurance, and other concerns:
Overall, it was a great event, with a great turnout and excellent audience participation and questions. I'm looking forward to the next one! Below are some still shots from the event.
- Dr. Paul Thomas with Plum Health DPC
Common Criticisms of Direct Primary Care
In this blog post, I'm going to list some common criticisms to Direct Primary Care and my responses to these criticisms.
In a traditional family medicine practice, each doctor typically sees a panel of 2,500 patients. If each patient comes in twice each year, that means roughly 100 visits each week, assuming that the doctor works 50 weeks each year, or roughly 20 visits each day. In Direct Primary Care, doctors reduce their clinic panel to 500 patients. Now, if each patient visits twice each year, the doctor will see 20 patients each week, or 4 patients each day. If each patient visits three times each ear, the doctor will see 30 patients each week, or 6 patients each day. This allows the doctor to spend up to an hour with each patient and use the remaining time in their schedule to answer phone calls, texts, and emails as well as handle the administrative duties that go along with running a Direct Primary Care practice.
The biggest criticism of doctors who switch from a traditional or fee-for-service practice to Direct Primary Care is this notion of patient abandonment. This means that if the doctor cuts down their practice from 2,500 patients to 500 patients, there will be 2,000 patients that are "abandoned" or without primary care services.
My response to this is simple: I will no longer perpetuate a bad system. In the current fee-for-service system, patients do not have enough time with their doctor for a thorough evaluation, for all of their questions to be answered, and to feel truly cared for. In the current fee-for-service system, doctors are rushing from room to room to room and are unable to provide the kind of high-quality care that their patients deserve,
In the current system, primary care doctors are marginalized and devalued, predisposed to burn out and leaning towards early retirement. Younger medical students see their burnt-out, grumbling, and overstretched attending doctors in Family Medicine and choose not to become primary care doctors in the first place. Why earn less than other specialties in a field that is less-than fulfilling?
Direct Primary Care doctors are fighting to make primary care relevant again, to restore the doctor-patient relationship, and to create value for patients in a way that the current fee-for-service system cannot.
There's an old adage: "take care of yourself so you can care for others", and it's something that primary care doctors have forgotten about. The expectation of the system is that we should work hard, keep our heads down, and not question the health care administrators who send an overwhelming volume of patients into our clinics each day.
But when we begin to sacrifice the quality of our work simply because we don't have enough time, it's time to take a stand and re-think our practices.
This brings me to the next criticism: how many conditions can a primary care doctor really treat? aka how much coverage can a family medicine doctor really provide?
When a well-trained family medicine doctor is able to practice at the top of their training, they are able to manage between 80 and 90% of all patient concerns. From sore throats, to blood pressure management, Pap tests, skin biopsies, abscess drainage, diabetic management, and beyond, family medicine doctors are able to care for a broad and diverse range of conditions.
The secret sauce in Direct Primary Care is the amount of time we are able to spend with our patients. If I have an hour, I can use it to drain an abscess, to talk about the efficacy of your antidepressants, to draw your blood for the lab work you need, to remove that ingrown toenail, to fully evaluate your vertigo, to evaluate your child's Vanderbilt scores for ADHD, to dispense the necessary medications and more.
In the current fee-for-service system, the expectation is that primary care doctors perform a cursory evaluation and then make a referral to a specialist. In the Direct Primary Care model, primary care doctors have more time to address concerns to the fullest of their training. And if that specialty referral is necessary, Direct Primary Care doctors have enough time to personally manage the transition of care, to make the follow up phone call and to get a full picture of what happened during that referral.
To summarize, Direct Primary Care doctors who leave the traditional fee-for-service system are not abandoning their patients. Rather, they are now free to practice medicine to the best of their ability by having enough time to give high-quality, thoughtful, and comprehensive primary care services to their patients. This will allow burnt out doctors to stay in practice for a longer period of time and it may inspire the next generation of medical students to choose primary care.
Thanks for reading, and have a wonderful day,
- Dr. Paul Thomas with Plum Health Direct Primary Care
You Should Own Your Health Information
You should own your information, especially when it comes to your health and wellness. Unfortunately, health care consumers don't have easy access to their own healthcare information, and this can lead to serious problems.
I firmly believe that you, the patient, health care consumer, or however you want to describe yourself, should be the sole owner of your healthcare information. When you visit a new doctor, you should take your health information with you, like a thumb drive or a credit card with an information chip.
With your permission, your doctor would review and evaluate you and your health information before making any treatment decisions. This would be closer to ideal than our current system in which healthcare systems or large hospital systems own your health information.
This may become problematic or even life threatening if your health records are kept with one hospital system, but you have to go to a different hospital system because of an accident or injury. Mistakes can be made if you lose consciousness and are unable to communicate your past medical history, allergies, and preferences.
Some hospital systems are beginning to allow patients access to their personal health information, but it is often through proprietary applications that may be difficult to navigate and even more difficult to share with different health systems or physicians.
In my practice with Plum Health Direct Primary Care, I consciously and deliberately share and make clear your health information. Of course, I only give you this information with your written permission. I share your information, lab results, diagnoses and treatment plans because it will allow us to make better decisions together.
I believe that when you are well-informed about your health status and equipped with the necessary information, we can make the best decisions about your health and treatment plans.
Furthermore, if you choose to seek a second opinion, the consulting doctor will have easy access to the information we discussed, and will therefore be able to make a better decision.
On a related note, I am really excited about the recent FDA approval for Direct-to-Consumer marketing of Genetic Health Information, namely 23andMe's Health + Ancestry product.
With only a saliva sample, 23andMe is able to produce a genetic health profile, with 10 potential genetic diseases including Alzheimer's Disease and Parkinson's Disease.
There are some pros and cons to this information. As I've stated above, with more information, you can make better decisions about your health care and how you want to live your life. On the down side, you may have a test with false positive or false negative results, or you may not understand the results at all.
In the case of a false positive, this would mean that you have tested positive for a condition that you may not have or may not develop. In the case of a false negative, this would mean that you have tested negative for a condition that you actually have or will develop.
These imperfections considered, I still think personal genetic testing will be a valuable tool as we move forward in this new health care ecosystem. It will enable patients and doctors to make better decisions about treatment. This is especially true as genetic profiles become more sophisticated and we may begin to learn how different genetic profiles are affected by different medications.
Thanks so much for reading and watching and have a wonderful day,
- Dr. Paul Thomas with Plum Health DPC
Plum Health out at America's Future Foundation Event
This week I was invited to speak at an America's Future Foundation meetup in Detroit. It was held at the Detroit Beer Company and the topic of discussion was free market healthcare. I was there representing Plum Health DPC and one of my colleagues, Chad Savage, MD of YourChoice Direct Care was there as well.
We talked for an hour about free market options for healthcare services in Detroit and Michigan, specifically Direct Primary Care. It was a great event and the audience members asked some great questions.
For example, people often ask about the difference between Direct Primary Care and Concierge Medicine. I wrote a blog post where I discussed the differences in detail, but in a Concierge Medicine Model, doctors charge a membership fee that is often greater than $100/month, continue to bill insurance for visits, and they do not typically offer money-saving ancillary services.
In contrast, Direct Primary Care doctors have membership fees in the $10 - $100/month range, do not bill insurance companies for services rendered, and typically offer money-saving ancillary services, like wholesale medications, at-cost labs and at-cost imaging.
Another common question about Direct Primary Care is about the legality of the practice. In 2014, Senator Patrick Colbeck spearheaded an effort in the Michigan Legislature to make Direct Primary Care "legal" in the State. I place "Legal" in quotation marks because it was not illegal before, but a grey area. Senate Bill 1033 of 2014 clearly defines Direct Primary Care and similar retainer-based medical services as legal in the State of Michigan.
Another common question is "how is this possible?", in reference to the savings on medication, labs and imaging services. As in, where does all that extra money go between the insurance-based prices for services and the direct prices? I often give examples of how I save my members on their meds, labs and imaging, and the attendees at this talk asked specifically about how I was able to save on these services.
It starts with wholesaling the medications and setting up contracts with independent retailers for lab services and imaging services. This way, we can negotiate at-cost pricing for services that you may need. These are often based on volume, so the more people who demand these services, the lower the overall costs. Then, I am not paying any middle men between these ancillary services and you the consumer. I do not mark up the prices on my meds, labs, or imaging services, because I want to provide you with the greatest amount of value for your healthcare dollar.
There were several other questions, but I will stop here! Again, it was a great meet-up and I'm looking forward to their next event! They have several chapters across the country, so you can see when and where their next events are happening on their Facebook page, just click "events".
- Dr. Paul with Plum Health DPC http://www.plumhealthdpc.com/
Direct Primary Care on NBC News
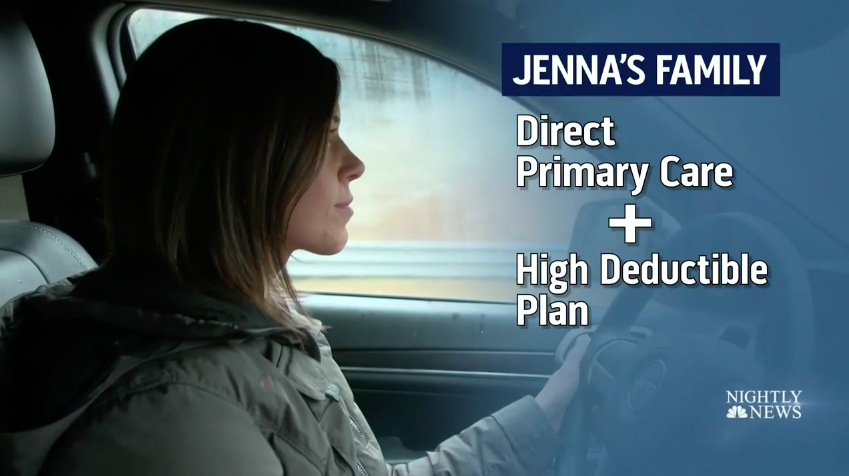
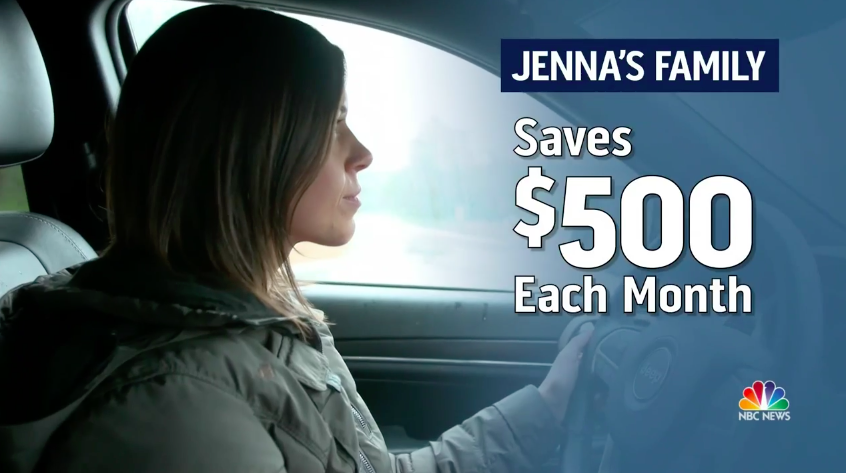
This week, Direct Primary Care was featured on NBC Nightly News with Lester Holt. If you are unfamiliar with this new model for healthcare delivery, Direct Primary Care is a membership model for healthcare that charges a relatively low fee for primary care services. The NBC News team starts out the piece by discussing the amount of time that the doctor is able to spend with the family, "maybe 30 - 45 minutes". At Plum Health, our visit time is about 1 hour for initial visits and 30 minutes for follow ups, so on par with what was stated in the video.
The video then goes on to discuss the benefits of Direct Primary Care with unlimited visits and the ability to text message the doctor for a flat, monthly fee. For most direct primary care doctors, patients are able to visit the doctor and have digital interactions with the doctor whenever necessary. At Plum Health, our patients can call, text, and email anytime and see us in the office anytime they need us.
The article then discusses the cost of the monthly membership, which is typically between $25 and $85 per month. In our case at Plum Health DPC, our prices are between $10/month for children up to $89/month for adults over 65 years of age. Young adults under 40 years old pay $49/month and adults over 40 years old pay $69/month. Direct Primary Care practices across the country typically fall in the $10 - $100/month range. Any monthly charges over and above $100 gets into the realm of Concierge Medicine. We wrote a previous blog post about the difference between Direct Primary Care and Concierge Medicine, here.
The NBC Nightly News piece goes on to discuss what's included in or what is covered by a typical Direct Primary Care practice. Typically, DPC practices cover unlimited primary care visits. At Plum Health DPC, our patients have unlimited visits with Dr. Paul, unlimited texting, emails and phone calls or unlimited digital communication. In addition, we charge at-cost pricing for routine lab tests and we charge wholesale prices for medications. Some doctors choose to include some basic blood work in the cost of the membership.
Because we don't charge an enrollment fee, we chose not to include basic blood work in our service. Instead, we perform at-cost labs at Plum Health. Complete blood cell counts are $4, Comprehensive metabolic panels are $6, Thyroid Stimulating Hormone tests are $6, Lipid panels are $6.55, and we have a modest draw fee of $2.
Families save money by choosing Direct Primary Care. The NBC News article discusses how the family featured in the video saves $500 each month by using a Direct Primary Care service and pairing that with a low premium, high-deductible plan.
This pairing of services is the ideal way to save money on your health care expenses. The issue that some people run in to is finding that Catastrophic coverage plan. Many of those plans have gone away after the Affordable Care Act was signed into law by President Obama. This is one of the many road blocks to wider implementation of Direct Primary Care plans. The other impediments include the inability to use Health Savings Account funds for DPC plans.
The next part of the article gets into the philosophy of Direct Primary Care. It talks about how Dr. Cunningham left a traditional family medicine practice. Now that he operates a Direct Primary Care practice, he sees fewer patients and makes less money. But, the income loss is worth it to him, so long as the insurance companies no longer dictate how he's supposed to take care of patients.
This part of the video touched a nerve with me. So often, we as doctors do not take care of our patients in the most optimal or ideal way because of the barriers put in front of us by insurance companies. By not accepting insurance company dollars, we are free to take care of patients in the way that they deserve to be taken care of. Dr. Cunningham says "It feels great to be practicing medicine the way it's supposed to be", and I agree!
Operating Plum Health DPC has allowed me to develop deep, trusting relationships with my patients that I never got to experience as a resident or in a traditional practice. The element that is so important to developing this relationship is time. When I am able to spend an hour with each patient during each visit, I am able to give them my full attention and deliver the kind of care that they deserve.
Dr. Cunningham, a Direct Primary Care doctor in Massachusetts, talks about how he is able to practice medicine the way he's supposed to be.
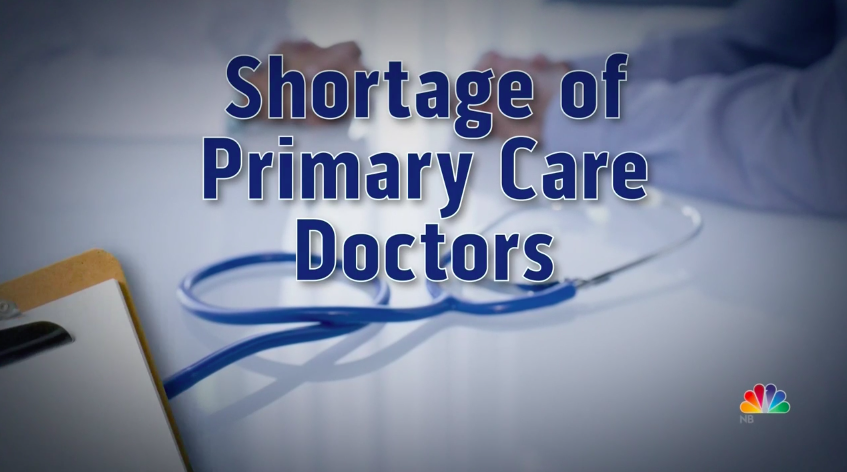
On the other hand, the article highlights the critical elements of Direct Primary Care: "Critics say there's already a shortage of primary care doctors". They don't really expound upon this thought or bring this thought to its logical conclusion, which is that if we already have a shortage of primary care doctors, then it is inexcusable for those primary care doctors to see less patients.
I take umbrage with this remark. There is a dearth of excellent primary care doctors because the practice of primary care medicine is one of the most challenging fields in medicine and it is often the lowest paid field in medicine. Medical students often choose higher-paying specialties in medicine that come with greater job satisfaction and less role strain.
I see the practice of Direct Primary Care as solving some of the issues with the current system. DPC medicine helps to eliminate the role strain that young doctors feel. When I have an hour to take care of a patient, I can really address them as a whole person. In the traditional or fee-for-service model, a primary care doctor has 10 - 15 minutes to address the whole patient, and this is nearly impossible. I've been there, seeing patients at this rate, and the best you can do is address 1 or 2 concerns before you have to move on to the next patient.
Direct Primary Care also can offer doctors a chance to earn a greater income if they have a panel of roughly 500 patients or members in their DPC practices. Some doctors choose to see less patients in their DPC practices, and therefore would make less money, but there is an opportunity to increase primary care doctors' salaries.
By eliminating the role strain that primary care doctors experience and by paying them a better salary, we can attract more medical students to primary care medicine fields like family medicine, general internal medicine, and general pediatrics. I take umbrage with the thrust that doctors should not see less patients because the system is broken.
It would be worse to see the system perpetuated with exhausted, frustrated, burnt-out primary care doctors seeing 2,500 patients each year. It would be better to have more medical students attracted to primary care fields, seeing 500 patients each year, limiting their role strain and increasing their incomes.
Another critique is that Direct Primary Care does not cover specialists visits or hospitalizations. I find this to be a moot point because the main thrust of Direct Primary Care is to deliver primary care services directly to our patients. We make no mention of Direct Specialty Care or Direct Hospital Care, and we make no attempt to promote these services in our offerings.
Too often, American consumers conflate "health care" with "health insurance", but these are distinct and separate services. You need to have health insurance, either a low-premium, high-deductible plan or a catastrophic coverage plan. This health insurance does exactly what the name implies: it insures you and your health against major, unexpected events.
Direct Primary Care, then, delivers the affordable, every-day primary care services that are needed by you and your family. You need to have primary care coverage, but you shouldn't have to pay an insurance company to pay your primary care doctor for what amounts to low-cost primary care services.
It makes sense to pay an insurance company to pay hospitals and surgeons for higher cost care, but it doesn't make sense to pay insurance companies to pay your primary care doctor for relatively lower cost primary care services.
As a side note, Plum Health DPC does offer specialists consultations for difficult clinical questions through our relationship with Rubicon MD. This allows us to ask about diagnostic testing, special labs to order, or to help us solve a difficult problem. But, as in the video, we do not offer specialists visits as a part of our service.
The closing thought from the NBC Nightly News video is that despite the drawbacks, it is worth it for some individuals and families to pay for Direct Primary Care services. As a Direct Primary Care doctor, the benefits are clear: you have a doctor on call for you any time you need it and access to time and cost-saving auxiliary services. The NBC reporter says that "Direct Primary Care is the answer, to save money and have a doctor who's always 'in'".
Thanks for reading and have a wonderful day,
- Dr. Paul with Plum Health DPC
Where the Bike Lane Ends
When I think about creating an affordable, accessible healthcare service in Detroit, there are many factors that I consider. One of them is physical accessibility by foot, by bike and by car. How can I help to ensure that all patients and community members have access to the resources that I provide in my Family Medicine practice? Am I able to serve the spectrum of people with varying incomes and abilities in my office? What barriers do people face when trying to get to my clinic?
Our Plum Health office is situated about 1 block from I-96/I-75 near the Vernor Highway exit. That's right, my office sits at the intersection of 2 "highways". Vernor Highway is not much more than one lane of each traffic in each direction, but the sentiment remains. We have a parking lot, there is sidewalk leading to our entrance, we are on a bus line, and we have parking spaces for persons with disabilities.
However, there is one area where we can improve! There is a Bike Lane on Vernor Highway in both directions that extends from SW Detroit and ends in front of my office in between 20th and 21st Streets. This is unfortunate, because there are Bike Lanes going in both directions on Michigan Avenue, less than 0.5 miles away.
All I'm saying is that there's a real opportunity here to connect SW Detroit, Mexicantown and the historic West Vernor Business District with Michigan Avenue, Corktown, and the Corktown Business District.
So for anyone in the City of Detroit, if you're reading/watching/listening, here's my prescription for a healthier road, healthier neighborhood, and healthier community:
- Clean up the garbage that has accumulated underneath the Michigan Central Station Rail Lines and along West Vernor highway. I'd be happy to help with this myself or by organizing a group of people in the community to assist or get this done. However, we would likely need support with some bulk collection if we went this route!
- Extend the Bike Lane on Vernor Highway between SW Detroit at 20th Street and Michigan Avenue. This would be relatively easy and would make for a safer crossing in the greater Roosevelt Park area.
- Cross walk markings in the Roosevelt Park area. There are several intersections in the Roosevelt Park area that are not demarcated by cross walks. This makes for dangerous crossings for pedestrians and bicyclists and ultimately less connected neighborhoods.
- Install lighting underneath the Michigan Central Station's viaduct.
Ultimately, citizens in Detroit face challenges with regular activity, obesity, and access to healthy food and parks. Creating an inviting environment for healthy activities by investing in Complete Streets at key intersections will be beneficial and will make an impact on the lives of residents in Detroit.
Sincerely,
- Dr. Paul with Plum Health DPC
How to Start A Direct Primary Care Clinic Right Out of Residency
This week, I received a question from one of my followers on YouTube! Big shout out to everyone who follows/watches - I appreciate you!
Anyways, the question is this: do you recommend starting a Direct Primary Care practice right out of Residency Training? And yes, I do! There are several ways to go about this, but it is better to start right out of residency than to wait until you have established fee-for-service patients or established insurance-based contracts.
Probably the best way to do this is to work for the first 6 months out of residence in an infusion center, urgent care, or hospital setting. Take one of these "moonlighting" jobs, work 40 - 60 hours a week, and spend the remaining 20 hours in your work week setting up your Direct Primary Care practice.
So, how do you set up a Direct primary care practice?
First, start with why. For more on this, read Simon Sinek's book of the same name. In short, you want to create a business that reflects your "why", or why are you doing this? For me, I wanted to create a healthy resource for the community that was affordable and accessible for all people. The name "Plum Health" reflects that mission. Plums are affordable and available to the community. You can buy them at nearby Eastern Market or from your local grocery store. They are also purple, representing inclusion, and health giving.
Then, develop a brand and a website. You want to create a sleek, modern website with an easy-to-pronounce name. "Plum Health DPC" works for me for the following reasons: Plums are healthy, kind of like "an apple a day keeps the doctor away". Plums can be drawn by making two overlapping circles, for me symbolic of the doctor-patient relationship, which has greater overlap in my practice. Also, Plum Health DPC indicates that we're a Direct Primary Care practice - it says so in our name! Finally, the domain "PlumHealthDPC.com" was available, which is a must!
Try to avoid stuff like "Salubrious Health" or some similar SAT vocabulary word. Also avoid overly long names. Keep it simple! Other alternatives that would have worked well for me would have been "Plum Primary Care" or "Plum Family Medicine". If you live in a small town or are in a distinct neighborhood, you can highlight that neighborhood or town in your name. I am in the Corktown/Southwest Detroit neighborhood currently, so something like "Corktown Primary Care" or "Corktown Family Medicine" would have been reasonable, with a domain name like "CorktownPC.com", "CorktownFM.com" or "CorktownMD.com". But, choosing the name is contingent on the availability of the domain.
The only downfall to naming your brand after a specific location is that if you decide to expand and open a second location, your brand will be incongruous with that second location. For me, I know that I wanted to be in Detroit to start and the goal is to expand regionally, so choosing a name that was not location-specific was important to me.
Your website is super important because it becomes a beta test for your market. If you are getting good traffic, engagement and responses from the community, these are positive signs. If not, it's not the end of the world, you may just have to be more proactive with your marketing efforts.
Beyond Naming, branding, and websites
Beyond naming and branding, form an LLC, PLLC, or S-Corp. Consult with a lawyer on which is best for you. Perhaps hire that lawyer or set up a retainer agreement so that you can consult that lawyer as your business grows. Then, set up a business bank account. Link that business bank account to software like QuickBooks so that your expenses are tracked.
Everything that you spend on the practice stays within the practice, meaning that you should treat your business as a separate entity from your personal finances. You may infuse your business with your own capital and that's why working 40 - 60 hours/week makes sense for 6 months. This way you can make enough money to fund your DPC start-up.
Alternatively, you can get a business or medical practice loan from a bank like Wells Fargo or Bank of America. Next, you need to have someone review your expenditures, so hiring an accountant or having a retainer agreement with an accountant is a must.
Choosing an Electronic medical record
Then, you should choose an Electronic Medical Record (EMR). Personally, I use ATLAS MD EMR because the platform is made by DPC doctors for DPC doctors. Also, ATLAS has a billing platform integrated into the EMR, which makes your life and your practice easier to manage. You can link your ATLAS MD account to your website and have people sign up directly on your site - these are called pre-enrollments. You can do this on a trial basis with ATLAS, and once you hit your start date, all those "pre-enrollments" will become paying customers when you hit "start" on the EMR side. At that point, your customers will start paying you for services and you will start paying ATLAS for the platform.
Other contracts
During this time, you should also be setting up contracts with your service providers. Internet, copy/fax machine, lab services, medication wholesaler, medical supplier, medical waste, shredding, general waste, etc... You should also be looking around for real estate options. A good way to test your model is to sublease from an existing doctor's office. Maybe you can find a general surgeon and you could sublease a few unused exam rooms - one to see patients and one to store meds, supplies, etc... If you are successful in that sublease location, you can look at expanding your business and setting up your own lease.
Benefits to subleasing are numerous. You won't have to set up your own internet provider, copy machine, medical waste, shredding, and general waste contracts - they will likely be included in your lease agreement depending on what you negotiate for.
Final thoughts
Setting up a Direct Primary Care practice is not easy, but it can be done successfully if you take measured risks as you grow. The website is your first test. For me, I started making house calls as a second test. As a third test, I subleased a one-room office from a local school. The next test for me will be to lease out my own office/building, and I'm just about at that point!
Also in this vlog, I touch on Public Service Loan Forgiveness programs and the effect it may have on primary care doctors choosing Direct Primary Care practices. More on NPR's website.
-Dr. Paul Thomas with Plum Health DPC
One last thing, if you’re a Primary Care Doctor or Allied Health Professional that is looking to Start and Grow a Direct Primary Care practice, check out our sister site www.StartUpDPC.com. You’ll find more information and in-depth courses on building the Direct Primary Care practice of your dreams.
Thanks for reading and watching, and have a wonderful day!
- Dr. Paul with Plum Health DPC
How Many Direct Primary Care Practices in Michigan?
The number of Direct Primary Care doctors in Michigan is difficulty to quantify. A reasonable place to start is with a definition of what Direct Primary Care is and is not. Philip Eskew is both a lawyer and a DPC physician over at DPC Frontier, and he sets forth a good criteria:
FOR THE PRACTICE TO QUALIFY AS A DIRECT PRIMARY CARE, IT MUST:
1) CHARGE A PERIODIC FEE
2) NOT BILL ANY THIRD PARTIES ON A FEE-FOR-SERVICE BASIS, AND
3) ANY PER VISIT CHARGE MUST BE LESS THAN THE MONTHLY EQUIVALENT OF THE PERIODIC FEE
I wanted to apply this definition to the State of Michigan, my home state, to see how many "DPC" practices meet this criteria. As far as pure Direct Primary Care offerings open to the public, there are two: Chad Savage, MD with YourChoice in Brighton and Plum Health DPC in Detroit.
There are other Hybrid DPC offerings within clinics that also bill third party insurance companies: Dr. Younes in Dearborn, Dr. Tindle in Grand Blanc, and Dr. Kevin Roy in Saginaw. I take issue with the Hybrid practices, because you lose the accessibility piece that makes DPC such a great delivery model - these doctors are still seeing a significant number of insurance-based patients and offering DPC to a subset of patients. So if a DPC patient needs to be seen, they "jump the line" and are seen ahead of the insurance-based patients. This is less than ideal.
Premier Private Physicians offers what I would define as Concierge Care or Concierge Medicine. The membership is $200/month or $2400 for the year and some labs and vaccines are billed to insurance companies. Visits are included, but they do not have contracts for at-cost meds, labs, or imaging because their patients are typically high income earners/wealthier people who are not as cost sensitive.
The other category of "DPC" in the State is employer-based DPC. Some large employer groups like United Shore have contracted with a "DPC" provider like SALTA or ProactiveMD to have on-site doctors to care for their employees. These practices are not open to the public and people who are not employees at these companies cannot access these services.
Because the access to care is limited, this operates more like a third party structure as the large company finds that it saves money to pay a capitated rate for each employee to an on-site doctor, rather than the patient using their employer-provided insurance to seek out urgent care or emergency services. Unfortunately, employees may start to use the "DPC" doctor more for urgent care type visits and less for primary care, chronic care, or preventive services.
If you wanted to include all of the above practices in the definition of DPC, there are roughly 8 "DPC" providers in the State of Michigan. My argument is that there are only 2 "pure" or authentic DPC practices in the State of Michigan. Sincerely, I would love to see more doctors taking the plunge into authentic DPC medicine, and am here to inspire, encourage, and consult other doctors to do just that.
If you want to add to the conversation or debate, please send me a message or write a comment below!
Thanks for your time,
- Dr. Paul with Plum Health DPC
Plum Health at Rock CF Rivers Half Marathon
This morning, I was out at the Rock CF River's Half Marathon and 5K in Grosse Ile, Michigan. Rock CF is an organization that advocates for patients with Cystic Fibrosis across the country, and their global headquarters are in Detroit on West Grand Boulevard.
Emily Schaller is the founder of Rock CF and organizes this race to raise money for the organization. The Rivers Half Marathon started at Grosse Ile Middle School and ran the perimeter of the island. The Rivers 5K started at the Grosse Ile Airport and ended at the GI Middle School.
I was representing Plum Health DPC as the race doctor and I was stationed at Mile 7.5/8ish. Fortunately, there were no major course injuries to report and things ran smoothly - no pun intended!
I'm really proud of the Rock CF organization, their mission, and the work that they do in the community. If you'd like to be a part of Rock CF and/or donate to people with Cystic Fibroses, hit up their website!
As a physician, I recommend 30 minutes of exercise each day for 5 days each week. That's about 150 minutes of exercise each week. Aerobic exercise like running a 5K is a perfect way to get and stay in shape. Exercise has innumerable benefits from better heart and blood vessel function to better control of diabetes, high blood pressure, and depression.
Now that the weather is nicer, it's the perfect time to develop healthy habits like running or walking every day. My pro tip is this: hang your workout clothes on your bed post and make exercise the first thing you do when you start your day.
To learn more about how you can become healthier, reach out to me here!
Thanks for reading and have a great day,
- Dr. Paul with Plum Health
Plum Health DPC in Grosse Pointe
On Tuesday night we were invited to speak to a group called the Eastside Republicans at the Grosse Pointe War Memorial in Grosse Pointe Farms, Michigan about Plum Health and Direct Primary Care.
Other speakers were Chad Savage, MD of YourChoice Direct Care and Senator Patrick Colbeck, a staunch supporter of Direct Primary Care in Michigan. This is a part of a tour across the State, a series of events across Michigan where Senator Colbeck and Direct Primary Care doctors talk about free market options in healthcare.
This was the largest crowd on this tour, and there were about 100 people in the audience. There were some great questions asked and good information shared about DPC, health shared savings plans, and unique solutions for employers.
The next event will be in St. Clair Shores on April 24th - mark your calendars!
Thanks for reading and have a great day,
- Dr. Paul with Plum Health
Medicaid Pilot Program in Michigan
Last week, we met up with Senator Patrick Colbeck in Lansing along with other legislators like State Representative Ned Canfield and other Direct Primary Care Doctors like Chad Savage of YourChoice Direct Care.
Currently, the State of Michigan spends 1/4 of the State Budget on health care programs like Medicaid. What I'm advocating for is better primary care and preventive services that create value for people in our State, that decreases costs over the long term by providing better care on the front end. The British say an ounce of prevention is worth a pound of cure, and by focusing more on primary care and prevention, I believe that we can take better care of our neighbors and save the State of Michigan money, money that can then be used to fix our infrastructure and spur economic growth and activity in our state.
Pragmatically, it may start with a Medicaid pilot program. Instead of giving Medicaid money to insurance companies to manage patients, that money is given directly to primary care doctors on a monthly basis to care for a panel of medicaid patients. The onus is then on the primary care doctor to provide excellent health care services for their community members and create more value and better health outcomes at a lower cost. I believe that this type of arrangement will allow for more holistic care, better access for patients, better outcomes, and cost savings.
I am excited about the prospect of this work and happy that we have some courageous leaders in this State who are willing to address these difficult problems head on.
Thank you so much for reading,
- Dr. Paul with Plum Health DPC