Plum Health Blog
New ICD 10 Codes for Long Haul Covid in Detroit
Different Types of long-haul covid syndromes that we see in our Plum Health clinic in Detroit
Many patients have been dealing with the fallout from their previous COVID 19 infections. Many of us know the symptoms of Coronavirus or COVID 19 infection - muscle aches, weakness, loss of taste, loss of smell, headaches, difficulty breathing, nasal congestion, and more.
However, not that many people know that COVID 19 can cause residual symptoms or lingering symptoms that can lasts for weeks, months, or even years after the initial COVID 19 infection. Patients can experience long-haul covid as residual covid symptoms like fatigue, muscle aches, muscle weakness, brain fog, etc..
Some patients can experience long-haul covid as POTS or Postural tachycardia syndrome (PoTS). With POTS, patients can have heart palpitations or rapid heart beats, they can become easily fatigued even after doing low or moderate intensity tasks, fainting or losing consciousness, or shaking and sweating. We’ve seen a handful of patients in our Plum Health DPC clinic with long-haul covid that presents as POTS.
Finally, we have had a few patients in our Plum Health clinic here in Detroit present with long-haul covid that presents as ME/CFS or Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. First, myalgic encephalomyelitis and chronic fatigue syndrome are commonly used labels for the same condition, so the names can be used interchangeably. I think these disease labels are combined with a slash to avoid confusion. Either way, ME/CFS is a condition that presents with a lot of fatigue or tiredness, difficulty sleeping or sleeping too much, pain, and often times brain fog. Symptoms are worsened when patients exert themselves - even a task like folding laundry can trigger profound fatigue.
ICD-10 codes for different long-haul covid syndromes
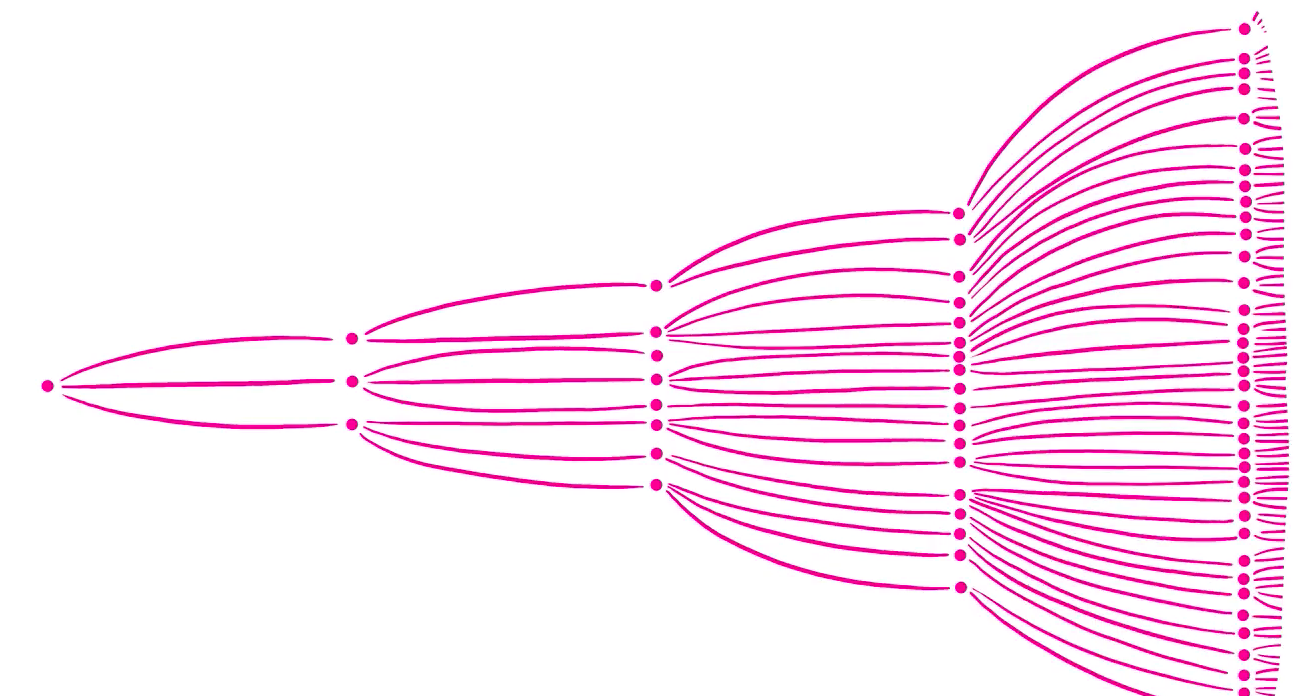
That being said, the ICD 10 or International Classification of Diseases, Tenth Revision, just released disease classifications for long-haul covid. See below, a tweet from Alexis N. Misko or @turnoftheshrew on Twitter:
Here’s a tweet from Alexis N. Misko or @turnoftheshrew on Twitter that shows the ICD 10 codes for different long-haul covid syndromes.
Those ICD-10 Codes are as follows:
U09.9 - Post-covid conditions unspecified
G90.A - POTS
G93.32 - ME/CFS
We take care of People with COVID 19 at Plum Health DPC
At Plum Health DPC, we take care of patients of all ages and stages. We also take care of patients who have Covid 19 or Coronavirus. We offer curb-side COVID 19 PCR testing and we also have antibody testing in the office. We have taken care of several patients with long-haul covid symptoms and as discussed above, we take care of patients with COVID who have POTS and ME/CFS presentations. We know that the mental, physical, emotional, and psychological strain of COVID 19 can be difficult to handle, so we pride ourselves on offering comprehensive care and timely referrals for folks who are struggling with long-haul COVID syndrome.
-Paul Thomas, MD with Plum Health DPC
Coronavirus Testing for Companies in Detroit
Coronavirus Testing for Companies in Detroit
At Plum Health, we offer coronavirus testing for companies in Detroit. We know that not every one of your employees wants to get the vaccine, but there are requirements for vaccination for many contracting jobs. For those employees who need weekly or twice weekly coronavirus PCR testing to help your company maintain compliance, we offer reliable testing in a convenient location.
Our office is located at 1620 Michigan Avenue, Detroit, MI 48216 and we are at the corner of Michigan and Trumbull in Detroit’s historic Corktown neighborhood. We offer walk-in testing at any time between 9 am and 5 pm. Our results are typically back in 24 hours, although some tests may take 48 hours to process. We offer weekly or semi-monthly invoicing to keep things simple for you and your company.
Please let us know if we can be of assistance in this regard.
- Dr. Paul Thomas with Plum Health DPC in Detroit Michigan
If you’d like to learn more info about this, please contact us by using the form below or by calling 313.444.5630.
At Plum Health DPC, we offer Coronavirus Testing to help your employees stay safe, healthy, and in compliance.
Coronavirus Vaccine Update for March 23rd 2021
Coronavirus status for march 25th 2021
I'm upset about this most recent spike in Coronavirus cases here in Michigan and Detroit/Southeast Michigan.
Yesterday, the State of Michigan reported 4,454 new cases, and sadly we are nearing 16,000 deaths from COVID.
We can do better. We all need to get vaccinated to protect ourselves, our loved ones, and our community. So far:
- 25.12% of Michiganders have received a single dose
- 14.31% of Michiganders have received both doses
That's great, but it will take 60 to 70% of us getting vaccinated to reach herd immunity.
I know that a lot of you are hesitant to get the vaccine, that's why I created this video and I answer as many questions as I possibly can to address these concerns. And, I'm happy to answer any other questions you have in the comments below.
Please - get the shot. You hold the power to save a life (or multiple lives) by getting vaccinated.
Coronavirus update march 2021
This is a presentation by Dr. Paul Thomas of Plum Health DPC in Detroit Michigan regarding Coronavirus, COVID 19, Coronavirus Vaccines, and frequently asked questions about COVD 19.
Topics:
Rising cases in Michigan, potentially due to lessening of restrictions
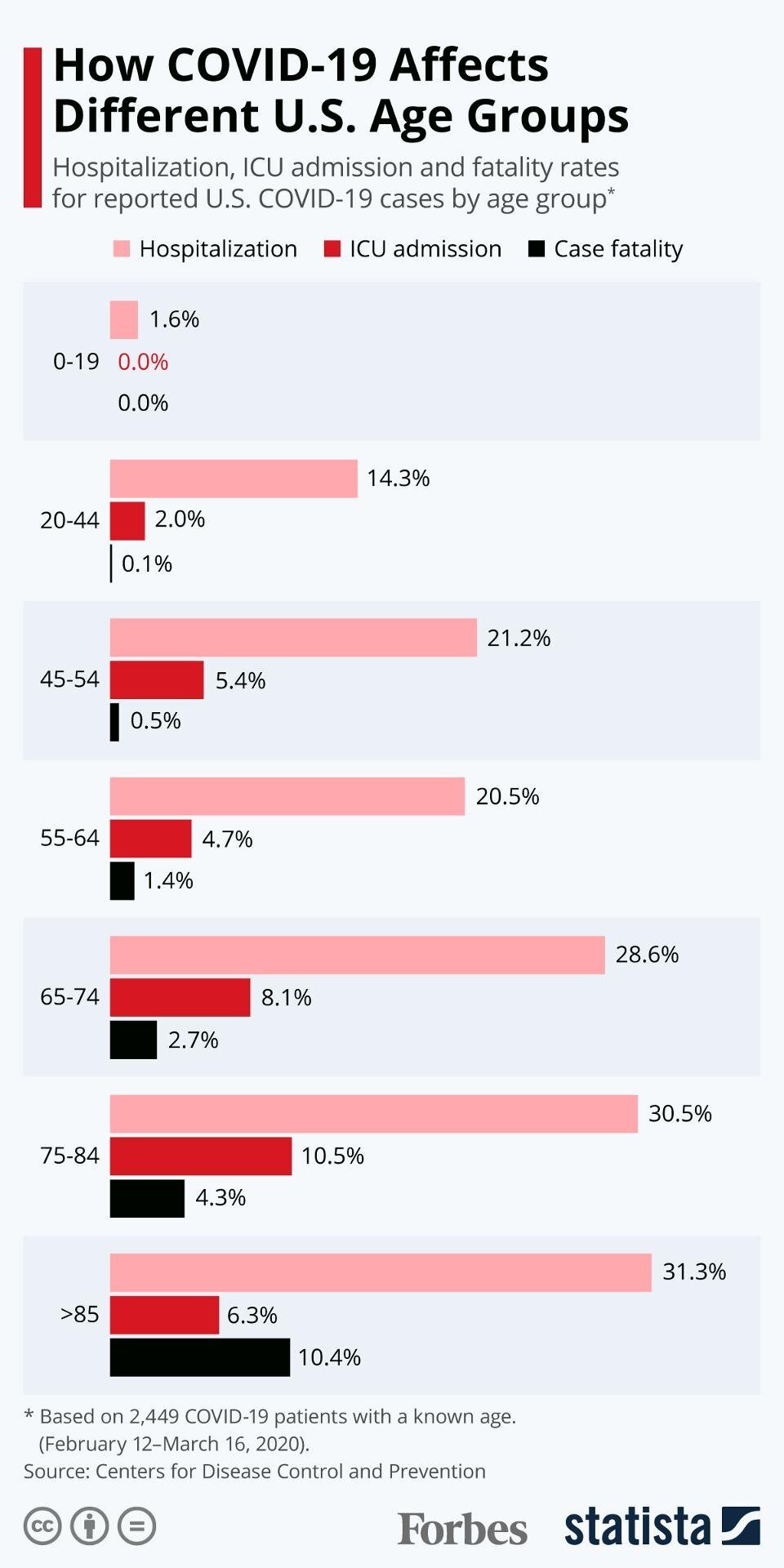
Age groups that are at the highest risk for Coronavirus
Comorbidities and Coronavirus, and why these pre-existing conditions lead to a higher risk of dying from Coronavirus
Hospitalizations and deaths related to coronavirus in the context of coronavirus and underlying medical conditions
How the mRNA vaccines work to create the Coronavirus Spike Protein
The difference between Pfizer, Moderna, and Johnson and Johnson Vaccines
What is the Adenovirus Vaccine Vector for the Johnson and Johnson Vaccine
Addressing a myth: the vaccine will alter my DNA - this is not true, the mRNA vaccine does not alter your DNA
Why the mRNA is easier and safer to produce and why it’s safer for patients
When will you get your vaccine? ie When will the coronavirus vaccine be available to me? (12:00)
Comparing and contrasting the Pfizer, Moderna, and Johnson & Johnson Vaccines
all of the vaccines are 100% effective in preventing hospitalization and death
The Johnson & Johnson vaccine is a 1 shot vaccine, so it may be better for specific populations
Comparing Polio to Coronavirus and Elvis Presley to Dolly Parton
How many vaccine doses have been given?
Is the Coronavirus Vaccine safe? (22:00)
If I’ve already had Covid, should I still get the Coronavirus Vaccine?
Should I get vaccinated with the coronavirus vaccine if I’m currently sick with Coronavirus?
Should I get vaccinated with the coronavirus vaccine if I’m currently pregnant or breastfeeding?
Vaccine efficacy against the South Africa and United Kingdom variants?
When will the Johnson and Johnson Vaccine be available?
What is Coronavirus Antibody testing (34:00)
What about myocarditis in college athletes who’ve had coronavirus?
Will there be a booster shot for Coronavirus vaccines?
What vitamins should you take to help ward off Coronavirus?
How common is Anaphylaxis after you get the Coronavirus Vaccine?
Can getting the Coronavirus cause problems with your immune system?
Thanks for reading and watching and have a wonderful day,
-Dr. Paul Thomas with Plum Health DPC
Coronavirus Update for March 2021 - Understanding the Vaccines
There are a ton of questions about the Coronavirus and what's going on with the virus and the vaccines in the City of Detroit and in Michigan, so I try to answer as many of those questions as I can in this video.
Low Rate of Pediatric Flu Deaths This Year
Did you know that there's only been 1 pediatric flu death this entire flu season? That's down from 150 to 200 pediatric flu deaths annually and it is likely attributed to mask wearing, physical distancing, and children being out of school.
Number of Coronavirus Cases in Michigan are on the Decline
In the State of Michigan, there have only been 1,400 new cases each day on average over the last 7 days, which is tremendous improvement from 9,000 cases each day in late November and early December 2020.
Coronavirus Death Toll in Michigan Hits a Grim Milestone
That being said, 15,610 Michigan residents have died from the coronavirus. To put that into perspective, there are 15,570 residents in Traverse City and 15,498 residents in Grosse Pointe Woods. To say that the coronavirus death toll is staggering is an understatement.
Coronavirus Vaccine Distribution in the State of Michigan
Fortunately, the vaccine doses are being distributed efficiently here in the State of Michigan and in the City of Detroit. 2.48 million vaccines have been given state-wide, and 8.92% of Michigan residents or 891,000 people have received 2 doses. Michigan ranks 9th in number of vaccines distributed nationally, and that's great.
How Does the mRNA Vaccine Work?
Next up, the Pfizer and Moderna Coronavirus Vaccine are made by injecting mRNA into your body, and that mRNA makes a spike protein which elicits an immune response from your body. People often think that the mRNA vaccine changes your DNA, but it doesn't.
Who is Eligible for the Coronavirus Vaccine in the City of Detroit?
Many more people are eligible for getting the coronavirus vaccine as time goes on. In Detroit, if your 50 or older with a pre-existing condition, you're eligible. If you're a food service worker, you're eligible. If you're a member of the clergy, a factory worker, a janitor, or a teacher, you're eligible.
You can see full details on who is eligible by going to this link or call 313-230-0505 Monday-Friday from 9 am until 6 pm to schedule an appointment.
The Johnson and Johnson Vaccine
The Johnson and Johnson vaccine is now available - it only requires one dose and it's a adenovirus vaccine, which means the vaccine is packaged in a virus vector. The J&J vaccine is 85% effective agains severe disease and 100% effective against hospitalization, and you only need one shot. If you're offered any of the available vaccines, get the shot, protect yourself, and protect your loved ones.
Stay safe and healthy,
- Dr. Paul Thomas with Plum Health DPC in Detroit, MI
City of Detroit Vaccine Rollout Update
The vaccine rollout here in Michigan has been relatively slow compared to other states. The Washington Post has a great article tracking vaccinations. Here’s where Michigan stands in the COVID vaccine effort:
At least 222,379 first doses have been administered (total population is 9.987 million)
covering 5.2% of the prioritized population...
and 2.2% of the state’s population.
Michigan has been allocated 696,600 doses,
enough to vaccinate 16.0% of the prioritized population...
and 7.0% of the state’s population.
On Monday, we received a press release from the City of Detroit about the Coronavirus Vaccine out of the TCF Center. Here it is, in full:
Statement from Detroit COO Hakim Berry on TCF COVID Vaccine Scheduling process
Since 9am this morning our COVID vaccine scheduling call center staffed by Rock Connections has experienced extremely high volumes, receiving more than 100,000 calls. Those who predicted that Detroiters would not be interested in receiving the vaccine were clearly incorrect.
Rock Connections has already increased its call center staff from 42 to 56 representatives booking the appointments. Call Center hours have now been increased by two hours a day and will operate 9 AM and 8 PM.
Our system is set up so that calls will not be kept on hold if there is more than a half-hour wait to speak to a representative. If your call is dropped, please call later today or anytime this week. At any point the wait time is under 30 minutes, your call will go through.
A major cause of call volumes is a large number calls from individuals who are not eligible. We do not have the capacity to answer questions from people under 75 or non-Detroiters about vaccinations in general. If you are not eligible to book the vaccine, please do not tie up the call lines.
As a reminder, people should call 313-230-0505 to schedule an appointment only if they meet the following qualifications:
A Detroit resident 75 and older
Any “good neighbor" 65 and older who drives a 75 year old (or older) Detroit resident to TCF
The following Group B essential workers: K-12 teachers and support staff and child care workers
We are booking 20,000 appointments through February 5th. The call center has the ability to book up to 4,000 appointments per day, so we expect to be booking appointments at least through the end of the day Friday. We will add to those appointments as fast as the federal government provides vaccines.
We thank Detroiters for their patience in this process and, most of all, for their commitment to being vaccinated so life can get back to normal as soon as possible.
This is somewhat frustrating, because the listed qualifications above are narrower than what was previously released. The previous statements from the State of Michigan include more people in the Phase IB, but the City of Detroit must be focusing on Group A only at this time, which includes only seniors over the age of 75:
Group A:
Persons 75 years of age or older not covered in Phase 1A.
This includes those in a congregate setting that were not reached in Phase 1A.
Henry Ford Health System Vaccine RollOut
Henry Ford Health System is also rolling out the vaccine here in Detroit, so if you have a MyChart account with Henry Ford, you could potentially receive an email from Henry Ford Health System (HFHS) about this vaccine option. See below for full details - this information was sent out to HFHS staff on January 8th.
What’s interesting to note is that Henry Ford is following the State of Michigan guidelines for eligibility, including “anyone 65 years and older and a broader category of essential workers.”
We have made considerable progress vaccinating our team members, having administered first doses to nearly 17,000 employees, with second doses underway for those vaccinated during our first days of the campaign. We are now expanding eligibility to volunteers, Henry Ford retirees 65 years and older, and approximately 3,000 students from our clinical education community. Additionally, we are partnering with multiple leaders across our region in a collaborative effort to vaccinate private practice physicians and other healthcare workers.
As you likely know, the state of Michigan has also expanded guidelines for eligibility to include anyone 65 years and older and a broader category of essential workers. Based on that guidance, we are finalizing our plans to begin vaccinating patients and members that meet those guidelines beginning next week.
Sites: We plan to launch two types of sites over time – those that will operate from our existing primary care clinics and others designed to serve as “mass vaccination sites” to accommodate larger numbers of patients safely, provide greater access and parking, and operate without disruption to our normal clinical activities. Here’s a breakdown by market:
South - The K-building at Henry Ford Hospital will open Monday, Jan. 11, with Henry Ford Medical Center – Ford Road expected to open by the end of next week
North - Three sites are expected to open by the end of next week: Henry Ford Medical Centers Lakeside and Columbus and the HAP Troy administrative building
Central - Two sites are expected to open next week: One Jackson Square as early as Monday, Jan. 11, followed by Henry Ford Allegiance Specialty Hospital, the current site for drive-through testing
Staffing: We know staffing continues to be a challenge but we have identified a number of viable options including our own primary care team members to staff the medical center locations. Additionally, HR plans to activate our central staffing model early next week to help identify needs, as well as team members who may be able to redeploy.
Scheduling & Patient Engagement: Initially, we will need to prioritize existing Henry Ford patients 65 years and older and plan to contact them proactively via email, providing resources to help them make an informed decision and encouraging them to sign up for MyChart if they haven’t already, for online scheduling when appointments become available.
We know that much of this is new territory and we will need to be agile as things change. A complex, community-wide vaccination campaign of this size and uniqueness requires unprecedented partnership, innovation and determination. We can’t imagine pulling this off with any other team and we are so proud of your efforts in service to our communities and each other.
Thanks for reading, and best of luck navigating these vaccine resources.
-Dr. Paul Thomas with Plum Health DPC
Frustrations Around Vaccine Rollout are Palpable
As we learn more about Coronavirus Vaccine availability, we'll keep you updated.
Vaccine Options for Oakland County Residents
For residents of Oakland County, there are some options, but they are not robust at this time.
One option would be the Oakland County Health Department. It looks like they are not yet vaccinating https://oaklandcountyvaccine.com/eligibility/
You could periodically check this website to see when they are opening up mass vaccinations.
The other option would be Beaumont Health. However, their website crashed on Friday from people trying to make appointments.
You could try to create an account via the MyBeaumont Chart, here: https://www.beaumont.org/my-beaumont-chart and hope that they send an email to you.
Some of our patients have received an email invitation via the Beaumont MyChart system to get the vaccine. They are trying to give it to people over 75 and then over 65 years of age.
Henry Ford Hospital is doing something similar. Here’s some information from the Detroit Free Press:
Don't call us. We'll call you.
That's what the state's COVID-19 vaccine website and many local health departments are telling seniors, teachers, child care workers and law enforcement officers who will be eligible starting Monday for coronavirus vaccines through an expansion of the statewide immunization program.
In part, that's because local health officials had almost no heads up before Gov. Gretchen Whitmer announced anyone 65 or older would soon be eligible to be vaccinated.
Whitmer announced Wednesday that starting next week, people in Priority 1B group will be able to get COVID-19 vaccines along with health care workers, people living and working in long-term care facilities and emergency medical responders who are part of the 1A Priority group.
In short, a lot of people are feeling frustrated and confused about the vaccine roll out - you're not alone in this.
As we know more information, we will share it with you.
As an addendum, in yesterday’s blog we talked about the Vaccine Rollout at the TCF Center in Detroit. Some of our patients have been calling the number since 9 am and it has been continually busy. If you get through, please send me an email or drop a comment on the bottom of this post.
- Dr. Paul Thomas with Plum Health DPC
Coronavirus Update with Daily Detroit and Dr. Paul Thomas
This week, we had a great conversation with Jeremiah Staes of Daily Detroit about where we stand in terms of the Coronavirus, the number of infections, the number of deaths, and the status of the vaccine.
Will There Be Another Spike in Cases After the Holiday Season?
There were 8 million travelers who flew during the holiday season. It’s possible that we may see a large spike in new cases after the holiday break as more people visit friends and family out of state, contract the virus, and bring it back to Michigan. We may see a lag in this spike as people tend to be busier around the holiday season and this can cause people not to want to visit the doctor’s office to get tested during this time. So, we shall see what happens.
Can I Work Out at the Gym During the Coronavirus Pandemic?
Just because a place is open, it doesn’t mean that it’s a great place to hang out at. This definitely applies to gyms, as gyms are a great place to pick up the coronavirus. In the gym, people are touching multiple surfaces, breathing heavily, and coming into close contact. Just think of all of the surfaces inside a gym locker, or a treadmill, or an elliptical machine, or a rack of weights. It’s virtually impossible to wipe down every single surface after every use, so it’s best to exercise outside or at home.
We Discuss Equitable Vaccine Distribution
More vaccine doses have gone to
Fighting for Equitable Vaccine Access in Detroit
Vaccine Distribution Challenges in Detroit
This week, we’ve been frustrated by the way the Coronavirus vaccine has been distributed. Large hospital system primary care doctors, who mostly operate in suburban communities, have been able to get vaccinated. Meanwhile, independent primary care physicians, including our staff and other neighboring Detroit-based primary care doctors, have struggled to gain access to the vaccine at this time.
The issue is that, in our region especially, there is a corporate-based vaccine distribution. The majority of the vaccine has gone to large corporate health systems, and those doctors, nurses, and support staff who are employed by those larger health systems are more likely to get vaccinated.
This is a big frustration because this inequity in vaccine distribution will likely trickle down and affect our region negatively; suburban folks who live closer to larger health systems may have easier access tot he vaccine than those residents in urban underserved communities.
We recently talked to the news media about this issue, and we’re grateful to Ross Jones and Channel 7 Action News for picking up the story.
A National Perspective
On a National level, doctors have expressed frustration to National Public Radio (NPR) about inequality of vaccine distribution within the hospital. The article states that:
“At hospitals in Massachusetts, New York, Arizona, California and elsewhere, medical professionals say that those with the most exposure to COVID-19 patients are not always the first to get vaccinated. And others who have little or no contact with COVID-19 patients have received vaccinations.”
Possible Solutions
What could solve this issue? Perhaps we could have a national database for people to sign up, to ensure that no one is missed in vaccination and that no one receives too many doses or too few doses. Because vaccine recipients are given a plain card with the vaccine date and a follow up date, I could see the vaccine distribution becoming a problem for those with low health literacy, mental illness, or memory problems like Alzheimer’s disease.
Additionally, we could ensure that there is more equitable vaccine distribution among local health departments and hospital systems. For profit hospital systems will always act in a self-interested manner, vaccinating their employees and patients first. Health departments are more likely to reach out to the highest risk populations in the community and deliver the vaccine to nursing homes, assisted living facilities, vulnerable populations, and community-based primary care offices.
For example, my colleagues in other states and other counties have received phone calls and invitations for vaccines at their local health department. Other regions have hospital systems that act in a more equitable manner, inviting physicians and support staff and high risk populations from the community to get vaccinated at that hospital system.
Why Vaccine Distribution Matters
While I understand that this coronavirus pandemic is a once-in-one-hundred-years type of event, I will never stop advocating for health equity, especially at the community level. Vaccine distribution shouldn’t be based on which individual or corporation has the most money, but it should be based on risk factors and need. Equitable vaccine distribution matters, and we’ll keep pushing for that ideal.
Thanks for reading and watching,
-Dr. Paul Thomas at Plum Health DPC
How To Prepare for the Holidays During the Coronavirus Pandemic
As winter approaches with COVID cases surging, taking steps to keep yourself and your loved ones both physically and mentally healthy is of paramount importance.
Get a Flu Shot
First and foremost, those who are able should receive the annual influenza vaccine as soon as possible. The CDC defines flu season as the period from December to January, meaning the peak for influenza cases this year is rapidly approaching.
While the flu shot will not specifically protect you from COVID, the vaccination confers a host of benefits, including reduced likelihood of hospitalization or exacerbation of chronic diseases such as COPD, diabetes, or heart disease. Reducing hospitalizations can relieve some of the burden on our already-strained hospital system as we contend with the rising number of patients with COVID.
For context, influenza caused 38,000,000 symptomatic illnesses, 18,000,000 medical visits, 400,000 hospitalizations, and 22,000 deaths in the United States during the 2019 to 2020 flu season. If everyone got a flu shot prior to this season, we could see a dramatic reduction in these numbers.
Winter Holiday Planning
Another consideration is planning for the winter holidays and the gatherings that tend to accompany them. As the cold weather drives more people inside and impairs the ability to gather outdoors, we expect to see the number of COVID cases increase markedly.
This is obviously a touchy subject; this has been a stressful year, and most of us want nothing more than to spend time with our friends and families. A strong social support network lowers stress, promotes good mental health, and can even lower your blood pressure.
While these benefits from social support systems are certainly desirable, steps should be taken to ensure everyone can enjoy the festivities without increasing the risk of getting sick. The current statewide restrictions limit indoor gatherings to a maximum of 10 people and no more than two households, so it is important to plan accordingly.
To maximize safety, anyone you invite should be practicing safe habits, including wearing a face covering like a mask, maintaining physical distancing at 6 to 10 feet at all times, and washing their hands regularly, prior to coming to the event to reduce the likelihood of catching COVID from community spread.
If there is any doubt as to whether someone may have acquired coronavirus before coming to your house, there are many sites where free testing is available, including the City of Detroit testing site at the Joseph Walker Williams Community Center on Rosa Parks Boulevard and most commercial drug stores like Walgreens and CVS.
If you test positive or test negative and have symptoms highly suspicious for COVID, including fever, dry cough, and loss of taste or smell, the safest course of action is to stay home and self-quarantine for 10 days. The worst case scenario would be to spread coronavirus from yourself to an older, sicker, or more vulnerable member of your family who could die from COVID or suffer significant physical impairments from the virus.
At the gathering, try to maintain physical distance as much as possible, wash your hands frequently, avoid sharing utensils, and consider shortening the duration of the event, as longer time spent indoors is associated with a greater risk of spreading the virus.
How a Healthy Lifestyle Can Help
Finally, try to maintain your regular healthy lifestyle habits, even during the winter months. If you typically exercise outside, dress in layers and ensure you are well-hydrated. Do your best to get eight hours of sleep each night, and practice healthy eating as much as possible.
There is always the temptation to overeat during the holidays, so conscientious eating and portion control can help reduce excess calorie intake and still allow you to enjoy your favorite holiday dishes.
The changes in weather and lack of sunlight can also trigger or worsen depression in some individuals, so it is important to communicate with your primary care physician about any depressive symptoms you may be experiencing. In general, it is good practice to keep in touch with your primary care physician, as they are best equipped to manage your healthcare concerns.
For those without a Primary Care Physician, my practice, Plum Health DPC, is currently accepting new patients. We offer subscription-based care and affordable testing and medications, including flu shots and COVID antibody testing. Anyone interested in signing up or seeking additional information can visit our website, here.
Thanks for reading and watching,
-Dr. Paul Thomas with Plum Health DPC, written with Geoffrey Ginter, Third Year Medical Student at Wayne State University School of Medicine
Coronavirus Update for August 2020 in Detroit
This is Dr. Paul Thomas with Plum Health DPC https://www.plumhealthdpc.com/ and I'm giving a Coronavirus Update for August 2020.
What's up with the spikes of cases in Oakland and Macomb County recently? It's likely that people are gathering for big events (I'm looking at you Jobbie Nooner, 43rd Port Huron Float Down, and the unofficial Woodward Dream Cruise) and not wearing masks or maintaining social distancing.
Stay safe. Wash your hands. Wear a mask. Protect yourself, your loved ones, and your neighbors, near and far.
#PlumHealth #CoronavirusUpdate #DirectPrimaryCare
Help Protect Other People From Coronavirus, Wear A Mask
How can you help protect yourself and other people from coronavirus? Wear a Mask
This week, Daily Detroit asked me a ton of questions about the Coronavirus and how to protect yourself, your family, and your community from the spreading virus. It boils down to wearing a mask. I answer many other questions during the podcast, listen here:
Why Should I wear a Mask?
You should wear a mask to prevent the spread of coronavirus. Here’s why:
Coronavirus has a long incubation period. People can have the virus without knowing it or having symptoms for about 4 to 5 days on average. This 4 - 5 day period of having the virus without showing symptoms is known as the incubation period. Some people can be in this incubation period for up to 14 days! Therefore, you could be walking around, infected with coronavirus and unknowingly spreading the virus to your friends, family, coworkers, and vulnerable people in your community. This is the main reason why you should wear a mask.
Coronavirus does not always cause symptoms. For COVID-19, data to date suggest that 80% of infections are mild or asymptomatic, 15% are severe infection, requiring oxygen and 5% are critical infections, requiring ventilation. So, in most cases, if you get the Coronavirus, you’ll be asymptomatic. If you’re asymptomatic, you can still spread the virus, so it’s important to wear a mask to prevent spreading the virus to your close contacts.
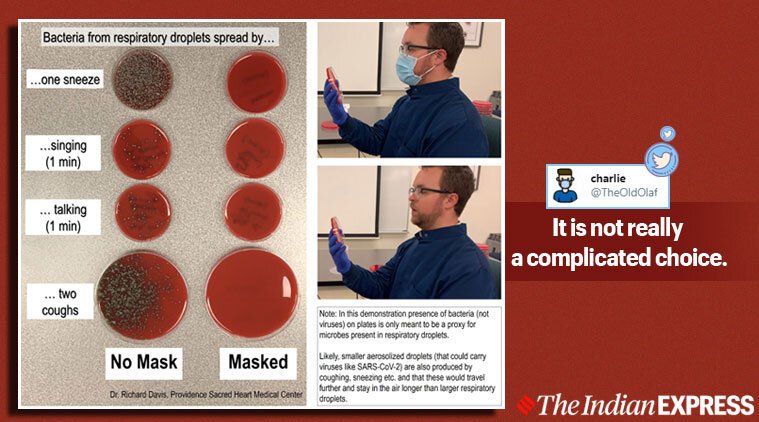
Wearing a mask prevents you from spreading the virus via respiratory droplets. When you talk, cough, sneeze, sing, yell, or breathe, you give off tiny respiratory droplets. These droplets carry the coronavirus and can land on surfaces or land in the noses or mouths or eyes of your close contacts. Wearing a mask puts a physical barrier between your nose and mouth and those around you, and therefore decreases the spread of droplets and the spread of coronavirus. If you want to explore this further, check out this blog post from Indian Express. Briefly, if you wear a mask it reduces the amount of bacterial and viral particles that you expel from your mouth when talking, as demonstrated in this image.
This PhD Scientist demonstrates bacterial growth related to wearing a mask vs not wearing a mask.
Why are bars being told to shut down?
Many bars in Michigan are closed or being ordered to close after outbreaks of coronavirus. There are four big reasons why bars are the best places to get coronavirus:
People drink at bars, and it’s difficult to wear a mask while drinking. Without a mask, it’s easier to spread Covid 19.
There tends to be loud music at bars, so people tend to raise their voices and speak more forcefully. This forceful speech tends to spread more respiratory droplets, which leads to an easier spread of coronavirus.
People tend to get closer to one another at bars - the less physical distance between people, the easier it is to spread Covid 19.
Bars are enclosed, intimate spaces, usually with poor ventilation. Many bars are windowless with low ceilings and poor ventilation systems. This can serve as a great space for a virus to circulate.
This is why bars like Harper’s in East Lansing have seen outbreaks of Coronavirus.
Here’s what Daily Detroit had to say:
Welcome to the holiday weekend, everybody. This is certainly a strange one, with coronavirus numbers once again on the upswing in Michigan and across much of the country, adding a complicated wrinkle to what is normally one of the busiest travel weekends of the year.
On today’s show, we make a house call to our friend Dr. Paul Thomas, founder of Plum Health Direct Primary Care in Detroit, for help answering your burning questions about COVID-19. We talk face masks, whether it’s safe to eat at restaurants or fly on airplanes, what to make of coronavirus liability waivers and more. And we’ll remind you that if you’ve got health-related questions about coronavirus, send ’em to us at dailydetroit@gmail.com and we’ll do our best to include them in future episodes with Dr. Paul. You can even send us audio of your question and we’ll try to work that audio into the show.
Also, we talk the latest, dispiriting COVID-19 data from the state and how we’re holding up from a mental health perspective more than three months into this weird, horrible quarantine that unfortunately shows little sign of ending anytime soon.
Thanks for reading, and stay safe out there!
-Dr. Paul Thomas with Plum Health DPC
Coronavirus Update For Detroit Michigan: What Happens Next?
Current Number of Coronavirus Cases and Deaths in Michigan
Covid 19 has been with us for well over 2 months now, and here’s where we stand:
45,045 Cases in Michigan
4250 Deaths in Michigan
657 new cases today
71 new deaths today
Despite the high numbers of total cases (cumulative cases) and cumulative deaths, there is a distinct downward trend in new cases each day. This is great, and it demonstrates the effectiveness of increased testing, social distancing parameters, government interventions like shutting down bars and movie theaters, as well as limiting the capacity of restaurants.
Percentage of People Testing Positive for Covid-19 in Michigan
In Michigan, about 23% of those who have been tested have tested positive for Covid-19. From April 6 to April 27th, the average percentage of positive tests has declined from almost 40% to just over 16%, which is well above the World Health Organization's 3% to 12% recommendation, but moving in the right direction.
Comparing Coronavirus in Finland, Sweden, and Norway
Some groups in the United States have demanded a re-opening of the country, and some of those have pointed to Sweden as a model country. However, Sweden has had worse outcomes with Coronavirus than its neighboring Scandinavian countries.
Finland has 5,573 cases and 252 total deaths
Norway has 7,915 cases and 215 total deaths
Sweden has 23,918 cases and 2,941 total deaths
It’s important to understand what’s working and what’s not working globally so that we can inform our own public policy at the National, State, County, and City level.
When will the Coronavirus Vaccine Be Available?
The Coronavirus vaccine will likely be ready in late 2021. There are multiple phases and stages that the vaccine has to go through, and we’re near the beginning of that process.
What is Direct Primary Care?
Some of you have asked more about Plum Health and Direct Primary Care - we provide a membership model for health care and we believe that health care should be affordable and accessible for everyone. We take care of patients of all ages and stages, from across the metro region, and of varying insurance coverages (including uninsured and underinsured folks). We love saving people money on healthcare services and delivering excellent care and service for our members.
A Few Thank You Notes!
Thank you to Max and his team at Commonwealth Sewing Company for the work they’re doing around making masks in Detroit. Thank you to Tyson Gersh at the Michigan Urban Farming Initiative for delivering 100 KN95 masks to our office - we appreciate you! And thank you to the team at MI FACE SHIELDS for providing us with 60 face shields - this is just another way we can protect ourselves and our patients during this time.
Thanks for reading and watching - Dr. Paul Thomas with Plum Health DPC
Paul Thomas MD Interviewed on Model D Media
On April 7th, 2020, Dr. Paul Thomas was interviewed by Dorothy Hernandez during Model D Media’s Facebook Live stream. The topic was Coronavirus and how we are managing this pandemic in the Detroit community.
Here’s what Model D Media wrote about this:
Editor’s note: This guest column by Dr. Paul Thomas, a family medicine doctor and founder of Plum Health Direct Primary Care, has been adapted from this blog post on the health center's website. Click here for the full post published on April 4.
The COVID-19 pandemic has brought an overload of information — and there's a lot of misinformation out there. Do you have a question for Dr. Thomas about coronavirus? Join us on our Facebook page for a Facebook Live Q&A at 10 a.m. Wednesday, April 8, with Dr. Thomas.
Q: Which counties nationwide have been impacted the most by coronavirus?
A: From the perspective of the number of cases and the number of deaths, the following counties/areas have been impacted the most by the coronavirus:
New York City (Queens, Bronx, Manhattan, Brooklyn, Staten Island)
Wayne County, Michigan
King County, Washington
Orleans County, Louisiana
Cook County, Illinois
Oakland County, Michigan
Bergen County, New Jersey
This comes from the Johns Hopkins Coronavirus Resource Center and it's notable that Michigan has two neighboring counties in the top six hardest-hit counties: Wayne County and Oakland County.
Q: Why has Michigan and Southeast Michigan been hit so hard by the coronavirus?
A: Bridge Magazine wrote an excellent article on this and I agree with their assessment with one addition that we haven't been talking about.
In the article, Bridge Magazine talks about the following factors causing Michigan to be more susceptible to the virus:
Automotive trade with suppliers in Wuhan China
Detroit Metro Airport with Direct Flights to Wuhan, China
Michigan’s March 10th Presidential Primary
Ties between Detroit and Italy via Fiat Chrysler (FCA)
In addition to these factors, I would want to add a few others, including higher rates of overweight and obesity in Detroit and Michigan - rate of overweight is 47.5% in Detroit (34% in NYC) and rate of obesity is 34.6% in Detroit (22% in NYC).
All of these factors have led to a higher case fatality rate here in Detroit and Michigan than the national case fatality rate:
National case fatality rate is 2.47%
Michigan case fatality rate is 3.75%
Detroit case fatality rate is 3.29%
Q: What are the comorbid conditions increasing the risk of mortality in COVID-19 positive patients?
A: [Last] week, I spoke with a physician colleague at one of the nearby regional hospital systems and we discussed the conditions that lead to a higher mortality rate. These comorbid conditions are as follows:
Cardiovascular disease (High blood pressure)
Diabetes
Pulmonary Disease
Obesity
Cancer
These factors that we discussed were similar to those studied in Wuhan, China.
While it’s still too early to state exactly why this is the case, I have a few theories. First, African American folks have higher rates of diabetes, hypertension, and obesity than their white counterparts here in Detroit and in Michigan. As we stated above, these are risk factors for higher mortality from the coronavirus. Next, African American people may be more likely to depend on low and minimum wage jobs that put them at a higher risk of contracting the coronavirus.
Q: Should I wear a mask to prevent the spread of the coronavirus?
A: Yes, the CDC now recommends that all Americans wear a mask when in a place where they have a higher chance of contracting the Coronavirus, like grocery stores. This can be a cloth or fabric mask. Please wash these each day if you wear them. Please do not hoard surgical or N95 masks as these are needed at hospitals at this time.
Q: What can you do to slow down the coronavirus?
A:
Stay at home
Donate extra supplies to hospitals or your primary care doctor’s office
Unused N95 masks
Unused nitrile gloves
Donate blood
DO NOT congregate in large groups
DO NOT visit elderly or vulnerable relatives, even if you feel fine
Act as though you have the virus
Coronavirus Update: What's Up With Antibody Testing?
Coronavirus Update for Detroit Michigan
As of April 16th, 2020 at 3 pm, there have been 673,215 cases of Coronavirus in the United States and 34,384 deaths from the Coronavirus in the US. This is a case fatality rate of 5.1%.
There have also been 29,263 Total COVID-19 cases in Michigan and 2,093 deaths in Michigan, for a case fatality rate of 7.15%. Further, Detroit has seen 7,383 Coronavirus cases and 546 Coronavirus deaths, for a case fatality rate of 7.3%.
Racial Disparities in Health Outcomes for the Coronavirus
There have been and there continue to be racial disparities in health outcomes related to the Coronavirus. Here in Michigan, African Americans make up only 14% of our state population, but account for 41% of the deaths due to Coronavirus statewide.
Here in Michigan, African Americans make up only 14% of our state population, but account for 41% of the deaths due to Coronavirus statewide.
In other regions, the disparities are even more evident. In Chicago, where African Americans make up only 30% of the population, they account for 52.1% of the COVID-19 cases, and 68.6% of the COVID-19 Deaths. You can read more about Chicago specifically, here.
In Louisiana, the disparity is similar. Louisiana’s population is 33% African American, according to 2019 U.S. Census data. According to the Governor of Louisiana, 70% of Louisiana’s coronavirus deaths are African Americans.
In Chicago, where African Americans make up only 30.1% of the population, they account for 52.1% of the COVID-19 cases, and 68.6% of the COVID-19 Deaths. You can read more about Chicago specifically, here.
When these stats are brought up, some people point to disparities in underlying health conditions as the reasons for these disparities in death rates among African American communities. And yes, that is the point - there are huge underlying health disparities between African American people, Caucasians, and other minority populations, and if we as a society want to stop pandemics from disproportionately affecting minority communities in the future, we will have to work tirelessly to address these health disparities.
Comparing Coronavirus and Influenza
Both Coronavirus and the Flu are spread by droplets, but Coronavirus may also be airborne, making transmission that much easier for Coronavirus. The incubation period for Coronavirus can be 1 to 14 days. This makes transmission of the Coronavirus much easier because during that incubation, the person who is infected may not have any symptoms, but they may be infecting others by shedding virus. This paired with the Transmission rate or R0, leads to a greater rate of spread and infection. This is why our stay-in-place orders statewide here in Michigan are so critical - we’re saving lives by staying at home and preventing the virus transmission.
Unlike the Flu, there are no available antiviral treatments and there are no vaccines for the Coronavirus. For the Flu, we have Oseltamivir (Tamiflu) and the Flu Shot to help us treat and prevent the Flu from spreading, but we don’t have these options for Coronavirus.
The hospitalization rate is much higher for Coronavirus, at 12 to 20%, whereas the hospitalization rate is only 0.6% to 1% for the Flu. Death rates are also very high for the Coronavirus. As discussed above, the case fatality rate for the US is 5.1% and the case fatality rate for Michigan is 7.15%. This makes the Coronavirus 50 to 70 times more deadly than the Flu.
How Much Does Coronavirus Care Cost?
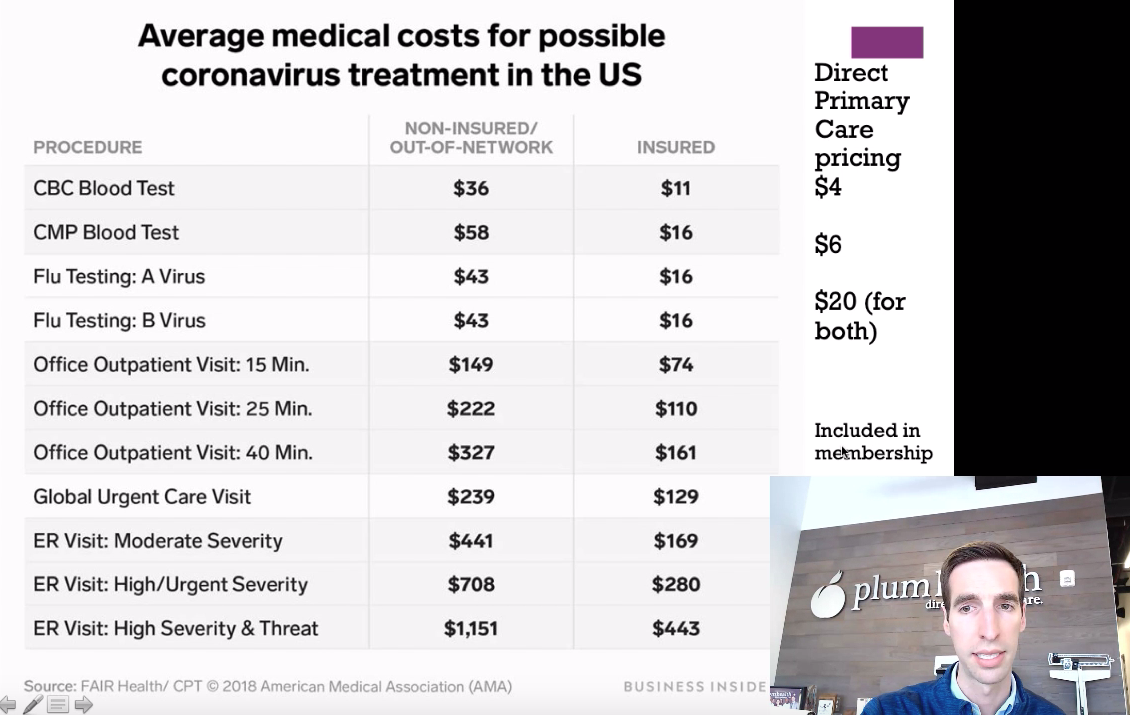
The President has worked with health insurance companies to make Coronavirus testing free, but there are other costs that patients incur when seeking care for the Coronavirus. If you’re uninsured, you can be charged $149 for a 15 minute visit with your doctor, $86 for flu A and flu B testing, and $94 for some basic lab work.
Compare that with the cost of care in a direct primary care practice, where you pay a monthly membership of $49 to $99 monthly and all of your visits - in person and telemedicine - are included in the membership package. The membership also allows you to get steeply discounted labs, medications, and imaging services.
Comparison of Coronavirus care costs between those who are uninsured, those who have insurance, and those who are members of a direct primary care practice.
What is antibody testing for Coronavirus?
Antibody testing will become increasingly important as we as a Nation confront and manage the Coronavirus pandemic.
Currently, we as a medical community are offering RNA testing, which involves a nasal swab or a posterior pharyngeal swab. This test helps us identify those who actively have the virus and are shedding RNA. This is a good test and it tells us who is actively infected with the Coronavirus. The downside to this test is that there is a relatively short window of time when this test will detect the Coronavirus.
Soon, more and more private labs and hospitals will roll out Coronavirus antibody testing. The procedure looks like taking a prick of blood from the finger and testing that blood for antibodies, or proteins that your immune system makes to fight off this virus. First, your body makes IgM, and then your body makes IgG. IgG gives you long-term immunity to the Coronavirus, and immunologists anticipate that we will carry this immunity for 1 to 3 years.
So, if you test positive for IgM, only, you likely have only recently recovered from Coronavirus. If you test positive for IgM and IgG, you may have had Coronavirus approximately 14 days ago.
The only downside to these antibody tests is that we’re relying on the test manufacturers to produce an accurate test. That being said, this is the best tool that we have right now to find out who has had Coronavirus and who has built a robust immune response to Coronavirus.
What Can you do to Prevent the spread of Coronavirus?
Stay at home
When you go outside of your home, wear a mask and keep 6 feet between yourself and other people. Only go to the grocery store once each week to minimize unnecessary contamination and spread of the virus.
Donate extra supplies to hospitals or your primary care doctor’s office - we currently are running low on masks, so if you have them, we would appreciate a donation to keep our staff, patients, and community safe.
Unused N95 Masks
Unused Nitrile Gloves
Donate Blood
Donate Plasma if you’ve had Coronavirus and recovered - your plasma could be used to save a life.
DO NOT congregate in large groups
DO NOT visit elderly or vulnerable relatives, even if you feel fine
Act as though you have the virus
Thanks for reading and watching, and have a wonderful day,
-Dr. Paul Thomas with Plum Health DPC
Dr. Raquel Orlich Featured on WDET's Detroit Today
This week, Dr. Raquel Orlich was featured on WDET’s Detroit Today radio program. Dr. Orlich answered many insightful questions from both the host Stephen Henderson and callers. To listen to the show, follow this link.
Raquel Orlich, DO is a board certified family physician. She has been with Plum Health since July 2019 and everyday she works to deliver affordable and accessible health care in Detroit. She is passionate about quality patient-centered care and establishing strong doctor-patient relationships. Her clinical interests include osteopathic manipulative medicine for chronic musculoskeletal issues, women’s health, and preventative health. She is a graduate of Michigan State University College of Osteopathic Medicine and completed her residency training at Ascension Macomb-Oakland Hospital.
Dr. Paul Thomas and Dr. Raquel Orlich are family medicine doctors with Plum Health DPC in Detroit Michigan. Recently, Dr. Raquel Orlich was featured on WDET to discuss Coronavirus.
Here’s the abbreviated transcript from WDET:
Guests
Dr. Anne Messman, emergency room doctor at a Detroit Hospital
Dr. Raquel Orlich, family doctor at Plum Health Direct Primary Care in Corktown, Detroit
I live alone and have been sheltering in place. Is it OK for me to visit other people who have also been sheltering in place by themselves?
No. The social distancing guideline still stands not to visit people. Until we know how to identify asymptomatic carriers, we must stay apart, unfortunately.
Do asymptomatic people ever show symptoms, or do they stay asymptomatic?
“Asymptomatic carriers, by definition, never get sick or show symptoms, but they can still pass on the virus,” says Dr. Messman.
Can COVID-19 survivors get infected by coronavirus after they have recovered?
We don’t know, yet. We do know the coronavirus has mutated several times, so, at this time, we believe it is possible that a survivor could get the virus again.
How long does it take for someone to shed the virus?
It varies greatly. Some people stopped shedding the virus soon after recovery, and for others, it took up to a month. We also don’t know yet if you can infect someone while you’re shedding the virus.
I was exposed to someone who later tested positive for coronavirus. I have had symptoms including a cough and low energy, and I passed out recently. What should I do?
Since there is still no treatment for COVID-19, if you are experiencing mild symptoms, it is best to stay home and recover. Do not take NSAID medications like ibuprofen or Motrin. It is okay to take Tylenol if you want to treat a fever. If your symptoms are severe and you need medical attention, you should go to the hospital.
I had a cold last month and some of those symptoms are still lingering. Is that a symptom of coronavirus?
If you’ve had a cold, or have had seasonal allergies in the past, don’t worry. A tickle in the throat can last weeks after having a cold. However, if you have symptoms that are unusual for you, pay attention for symptoms of COVID-19 and take extra care. If you experience sever symptoms, go to a hospital.
Does using Tylenol to treat a fever negatively impact my immune response? Should I just leave the fever untreated?
Healthcare providers have differing opinions on this question, but if you have a fever and want to treat it, Tylenol is OK. A very high fever can be very dangerous and should not go untreated.
Does wearing a mask protect me, or other people?
Wearing a mask protects both you and other people. The main function of the mask is to catch droplets from someone coughing or sneezing before they get in the air. It is best to wear a mask if you need to go out.
I had a stomach virus recently. Is that a symptom of COVID-19?
Some patients who tested positive have experienced symptoms like diarrhea or vomiting. There are other reasons you might experience gastrointestinal issues including influenza or food poisoning.
I may have been exposed to someone with COVID-19, but I’m showing no symptoms. Can I get an antibody test to find out if am an asymptomatic carrier?
We do not have an antibody test, yet.
This week, Dr. Raquel Orlich was featured on Detroit Today with Stephen Henderson. She was able to answer many listener’s questions about Coronavirus and Covid-19
Coronavirus Update for Detroit Michigan
My name is Dr. Paul Thomas and I'm a Family Medicine Doctor in Detroit, Michigan with Plum Health DPC and this is my update for the Coronavirus as of Saturday April 4th.
Which Counties Nationwide Have been Impacted the Most by Coronavirus?
From the perspective of the number of cases and the number of deaths, the following Counties have been impacted the most by the coronavirus:
New York City (Queens, Bronx, Manhattan, Brooklyn, Staten Island)
Wayne County, Michigan
King County, Washington
Orleans County, Louisiana
Cook County, Illinois
Oakland County, Michigan
Bergen County, New Jersey
This comes from the Johns Hopkins Coronavirus Resource Center and it's notable that Michigan has two neighboring counties in the top 6 hardest hit counties - Wayne County and Oakland County.
What are the current number of cases and deaths from Coronavirus in Michigan?
Currently, there's 12,744 Coronavirus cases in Michigan and 479 deaths from the Coronavirus in Michigan. What's most troubling about this is the rapid and almost exponential growth of cases here in Michigan. We've seen cases doubling every 2 to 4 days, and that trend does not look like it's slowing down any time soon. That's why it's so crucial that we socially distance our selves to stop the spread of the coronavirus from person to person.
The alarming increase in new cases is also why the CDC now recommends face masks for individuals in the community.
Why Has Michigan and Southeast Michigan Been Hit So Hard by the Coronavirus?
Bridge Magazine wrote an excellent article on this and I agree with their assessment with one addition that we haven't been talking about.
In the article, Bridge Magazine talks about the following factors causing Michigan to be more susceptible to the virus:
Automotive trade with suppliers in Wuhan China
Detroit Metro Airport with Direct Flights to Wuhan, China
Michigan’s March 10th Presidential Primary
Ties between Detroit and Italy via Fiat Chrysler (FCA)
In addition to these factors, I would want to add a few others, including higher rates of overweight and obesity in Detroit and Michigan - rate of overweight is 47.5% in Detroit (34% in NYC) and rate of obesity is 34.6% in Detroit (22% in NYC).
All of these factors have lead to a higher case fatality rate here in Detroit and Michigan than the national case fatality rate:
National Case Fatality rate is 2.47%
Michigan Case Fatality rate is 3.75%
Detroit Case Fatality rate is 3.29%
What are the Comorbid Conditions Increasing the Risk of Mortality in Covid-19 positive patients?
This week, I spoke with a physician colleague at one of the nearby regional hospital systems and we discussed the conditions that lead to a higher mortality rate. These comorbid conditions are as follows:
Cardiovascular disease (High blood pressure)
Diabetes
Pulmonary Disease
Obesity
Cancer
These factors that we discussed were similar to those studied in Wuhan China.
Why are African Americans disproportionately affected by Coronavirus?
African Americans in Detroit and Michigan have been disproportionately affected by the coronavirus. Even though African American people make up only 13.8% of the population in the State of Michigan, 35% of the Coronavirus cases and 40% of the Coronavirus deaths have been experienced in the African American community.
Coronavirus Cases by Race in Michigan. This according to Michigan.gov/Coronavirus. Note the higher rates of infection and mortality in the African American community relative to the population. African Americans make up 13.8% of the population in the State of Michigan.
While it’s still too early to state exactly why this is the case, I have a few theories. First, African American folks have higher rates of diabetes, hypertension, and obesity than their white counterparts here in Detroit and in Michigan. As we stated above, these are risk factors for higher mortality from the Coronavirus. Next, African American people may be more likely to depend on low and minimum wage jobs that put them at a higher risk of contracting the Coronavirus.
What is the Hospitalization Rate for Covid-19?
Currently, the hospitalization rate for Covid-19 is about 20% or only 1 in 5 people who get the coronavirus will require hospitalization. However, the rates of hospitalization increase with age, meaning that the older the patient, the more likely that they’ll need to be hospitalized for the Coronavirus. That’s why it’s so important to avoid visiting elderly and vulnerable residents in our community.
The older the patient, the more likely it is that they’ll require hospitalization for management of their Coronavirus infections.
Unfortunately, there is a very high mortality rate once a patient needs to be placed on a ventilator. According to studies out of Wuhan, China, the Mortality rate from Coronavirus is 62% among critically ill patients with COVID-19 and the Mortality rate from Coronavirus is 81% among those requiring mechanical ventilation. That means that if you require mechanical ventilation, only 1 in 5 Covid-19 positive patients will come off of the ventilator.
Limited Availability of Ventilators in Michigan Hospitals
The rapid increase in the number of coronavirus patients and the increasing demand for ventilators is putting hospitals, doctors, and nurses in a terrible situation. We’ve now reached the point where doctors are having to decide who lives and who dies from Coronavirus based on ventilator availability. I spoke with a colleague at a large hospital in the Detroit area who relayed that there were only two ventilators for the hospital remaining and that treatment decisions were being made based on comorbidities.
This is a very sad day because we should have never gotten to this point. If we had a functioning Federal Government with a coordinated response and if we had forward-thinking hospitals with greater capacity for disasters like this, we in the medical community wouldn’t have to be making these terrible life and death decisions based on lack of supplies and equipment.
Should I Wear a Mask to Prevent the Spread of the Coronavirus?
Yes, the CDC now recommends that all Americans wear a mask when in a place where they have a higher chance of contracting the Coronavirus, like grocery stores. This can be a cloth or fabric mask. Please wash these each day if you wear them. Please do not horde surgical or N95 masks as these are needed at hospitals at this time.
What can you do to slow down the Coronavirus?
Stay at home
Donate extra supplies to hospitals or your primary care doctor’s office
Unused N95 Masks
Unused Nitrile Gloves
Donate Blood
DO NOT congregate in large groups
DO NOT visit elderly or vulnerable relatives, even if you feel fine
Act as though you have the virus
Thanks for reading and watching, and have a wonderful day,
-Dr. Paul Thomas with Plum Health DPC
Can Vitamin C Treat the Coronavirus?
Can Vitamin C Treat the Coronavirus?
No.
At this time, there is no evidence that Vitamin C can prevent or treat the Coronavirus.
In late March, I began to receive an uptick in questions about vitamin supplementation. There is little to no evidence that high doses of vitamin C will prevent or treat the Coronavirus. But some people have been recommending these supplements as a panacea for all viruses and all seasonal afflictions. There’s also been a few social media posts promoting vitamin supplementation as a cure for Coronavirus. In this blog post, I aim to set the record straight on vitamin C and Coronavirus.
What is Vitamin C?
First of all, Vitamin C (ascorbic acid) is an essential nutrient as it supports normal growth and development and it helps your body absorb iron. Your body doesn’t produce or store vitamin C, so it’s important to get enough vitamin C by eating a healthy diet.
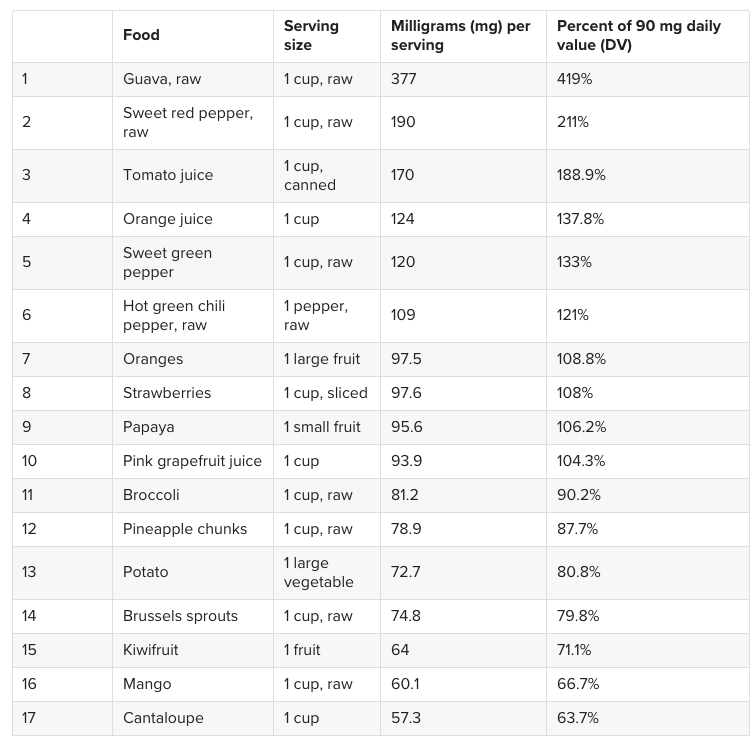
Next, and according to the Mayo Clinic, the average adult needs 65 to 90 mg of vitamin C each day. Again, we can get enough vitamin C by eating a healthy, well-balanced diet. There’s 190 mg of vitamin C in a raw sweet red pepper and there’s 97.5 mg of vitamin C in a large orange. Other foods high in vitamin C include guava, tomato juice, orange juice, strawberries, papayas, and broccoli.
Here’s an awesome chart from Medical News Today that shows which foods are rich in Vitamin C.
The best way to get enough Vitamin C? A healthy diet. The above foods have adequate amounts of Vitamin C.
Where is this Bad Advice on Vitamin C coming from?
Here’s the issue, in late March I was forwarded general advice from a holistic doctor who went so far as to recommend as much vitamin C “as your body can handle” but at least 3,000 to 5,000 mg each day. In their words, this would protect you from the Coronavirus.
Not only is this person misleading their patients and giving potentially dangerous medical advice on a non-individualized basis, but he is also profiteering on their lack of knowledge. The doctor has an online supplement store where patients can purchase his recommended vitamins without a prescription for a hefty sum.
This email was forwarded to me from a holistic doctor who has been prescribing the above supplements as Coronavirus “protection.” As a family medicine doctor who follows evidence-based guidelines, it is very frustrating to see this type of bad information circulating via email and on social media channels.
Can Too Much Vitamin C be Dangerous?
When people think of vitamins, minerals, and supplements, they think of good health. If supplements are good, then more supplements are better, right? But what people don’t know, and what this vitamin-pushing doctor should know, is that mega doses of supplements can have negative consequences.
Most adults only need 65 to 90 mg of vitamin C each day, and adults shouldn’t take more than 2,000 mg each day. Although too much dietary vitamin C is unlikely to be harmful, mega doses of vitamin C supplements might cause diarrhea, nausea, vomiting, heartburn, abdominal cramps, headaches, and insomnia.
Let’s create a hypothetical patient who is a middle-aged adult man who takes Metformin 500 mg twice daily for his long-standing diabetes. The Metformin works well, keeping his blood sugar and hemoglobin a1c levels near normal. It’s important to know that adverse effects of Metformin include diarrhea, GI complaints, nausea, vomiting, and abdominal distention.
If both the Metformin and the high-dose Vitamin C are taken at the same time, the side effects from Vitamin C supplementation may be incorrectly attributed to the Metformin, potentially causing the patient to stop a beneficial medication.
Always Talk to Your Doctor about Your medications and your supplements
It’s entirely possible that in some cases, a patient might be taking mega doses of vitamin C, and not inform their physician of these supplements. Usually a doctor only asks their patients about which medications they’re taking, and not specifically about supplements. If the doctor doesn’t know about these mega doses of vitamins, those adverse effects caused by the vitamin C mega doses may be blamed on or attributed to a life-saving or life-prolonging medications prescribed by your doctor.
And this is just one example - many medications, from blood pressure medications to SSRIs for depression to other medications for diabetes like glipizide can have gastrointestinal side effects. So, please, talk with your family medicine doctor or internal medicine doctor about the medications and supplements that you’re taking.
What Can You do to help improve your immune system?
Here’s my recommendation for a healthy lifestyle during this time:
Exercise: 1 hour daily
Sleep: 7 - 9 hours daily
Eat: a balanced, healthy diet
Meditate: 30 minutes to 1 hour daily
If you choose to supplement with Vitamin C, talk with your doctor.
As a final note, the USA Today wrote a good article about this topic, and Harvard Health has another good article about this topic.
Thanks for reading, - Dr. Paul Thomas with Plum Health DPC
Coronavirus Update March 26th for Detroit Michigan: Can you be Immune to the Coronavirus?
Coronavirus Update March 26th for Detroit Michigan
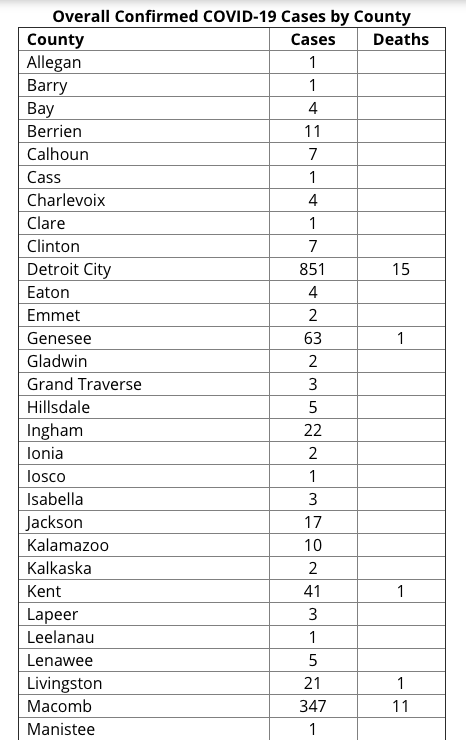
The Coronavirus continues to spread in Michigan. As of today at 2 pm, the Michigan Department of Health and Human Services has reported that there have been 60 deaths and 2,856 cases. That is a mortality rate of 2.1% as of today.
The Coronavirus is concerning for so many reasons, but the two biggest reasons are the rate of transmission and the mortality rate. The Coronavirus spreads, on average, to 2.5 to 2.9 people once an individual is infected. Also, the global mortality rate has been in the 3 to 4% range. Compared to the Flu, these numbers are staggering. The Flu has a rate of transmission of 1.3 and a mortality rate of 0.1%. That makes the Coronavirus 30 to 40 times more deadly than the flu.
Below are the number of cases by Health Department here in Michigan and the number of deaths by Health Department. Detroit is within Wayne County, but it has its own health department, so those numbers are separate from Wayne County Cases.
How Many People Have Tested Positive and How Many People Have Tested Negative?
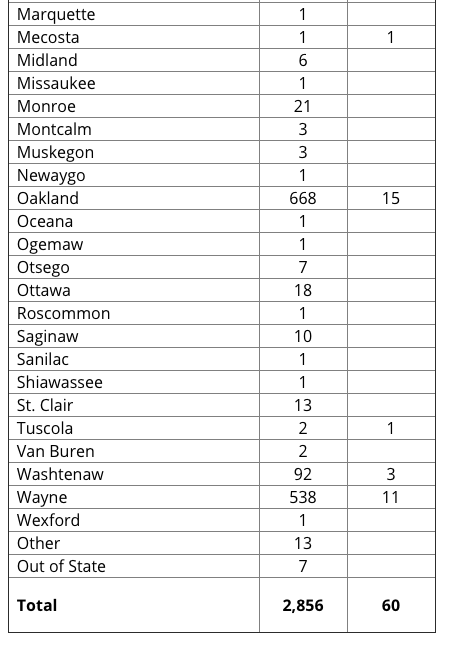
The State of Michigan today released their data regarding positive tests and negative tests.
30 of 744 outpatient tests have been positive, or a rate of 4.03% at the doctor’s office
1866 of 5261 hospital-based tests have been positive, or a rate of 35.4% at the hospital
557 of 3104 health department cases have been positive, or a rate of 17.9% at the health department
This tells us that if you’re well enough for your doctor to test you at the office and send you home, you are unlikely to have the Coronavirus. It also tells us that if you’re sick enough for your doctor to direct you to the hospital and you meet the testing criteria at the hospital (fever, cough, potential exposure), then you have a good chance of testing positive at 35.4%. This information can be found on the MDHHS Website.
Data from the Michigan Department of Health and Human Services showing the number of positive and negative tests in the State of Michigan as of 03/25/2020.
Hospital Beds are Filling up in Detroit
According to this article in the Detroit Free Press, the Beaumont Hospitals in Detroit and West Bloomfield are filling up with patients.
The health system is "facing limitations and nearing capacity with our testing, personal protective equipment and mechanical ventilators," said Beaumont Health Chief Operating Officer Carolyn Wilson. “We are taking steps to increase our capacity, such as converting some of our operating rooms into intensive care units.
“We have been actively transferring COVID-19 patients within our system to other Beaumont hospitals, as appropriate, if one hospital has more capacity than another."
According to this article in the Detroit News, Henry Ford Health System is facing the same challenges.
"Today our capacity is quite full at those two hospitals — West Bloomfield and Henry Ford Hospital in Detroit," said Dr. Betty Chu, associate chief clinical officer and chief quality officer. Chu is leading the health system's coronavirus response.
"We fortunately have the luxury right now of having additional capacity at some of our other campuses."
This is concerning because there are a limited number of staff, beds, and equipment to adequately are for Coronavirus patients here in the Detroit and Metro Detroit area.
As beds fill up and as our hospital personnel are stretched thin, we may be in a situation where doctors have to pick who lives and who dies simply based on issues of capacity. This is truly a terrible situation and one that we want to completely avoid.
That is why it’s so important to stay at home and avoid any unnecessary contact with people, by which you may become infected.
City of Detroit Will Begin Offering Free Coronavirus Testing Tomorrow
Unfortunately, the City of Detroit has been hit hard by the Coronavirus. But, Mayor Mike Duggan and the City of Detroit will begin testing people at the State Fairgrounds at 8 mile and Woodward to hopefully stem the tide. The aim is to test 50 people every hour and 400 people every day with this drive-through testing.
Testing is important because it can help us track the spread of infection and it can help people prevent the spread by self-quarantine if they find out that they are infected. You can learn more about this testing via the City of Detroit, here.
How Can I Become Immune to the Coronavirus?
Yes, you can become immune to the Coronavirus. When you get infected with the Coronavirus, your body will produce antibodies or immunoglobulins to the Coronavirus. First you’ll make IgM, and then IgG. This will confer long-term immunity to you.
Scientists estimate that you’ll be immune for 1 to 3 years based on previous infection and immunity rates from other Coronaviruses. This is why you can’t get re-infected by COVID-19. Once you have the virus, you’ll be immune to future infection.
This is important for several reasons. Over the next few weeks to the next few months, there will be a test of immunity. It will likely be a finger-stick blood test, using a drop of blood to measure the immunoglobulins like IgM or IgG to make sure folks are immune.
This will be especially important for doctors, nurses, hospital workers, and other critical staff. If we know that these folks are immune to Coronavirus, they can go back to treating patients with minimal risk of infection going forward. This test is pending as of now.
HOw will the Coronavirus Pandemic End?
The Coronavirus pandemic will end when we reach a Herd Immunity. Herd Immunity means that enough people in the population are immune to the Coronavirus, which will greatly limit its spread.
This Herd Immunity can be achieved in a few different ways. First, once a number of Americans get the Coronavirus, they will fight off the infection and become immune, limiting the spread of the virus once they recover. Second, once a vaccine is developed, many more people will become immune through vaccination.
Just like being vaccinated for the influenza virus or for Measles, Mumps, and Rubella, once you’re vaccinated for these viruses, your body creates immunoglobulins or antibodies to help protect you from infection from these viruses.
Unfortunately, the Coronavirus or COVID-19 vaccine will take 18 months to 2 years to develop, so this option will take a long time to achieve.
This image demonstrates Herd Immunity. The left hand panel shows what we’re dealing with right now with the Novel Coronavirus or COVID-19. No one is immune to this COVID-19 yet. The right hand panel shows Herd Immunity. The yellow figures are immune to the virus, so the spread of the virus will be limited. Herd Immunity defined: the resistance to the spread of a contagious disease within a population that results if a sufficiently high proportion of individuals are immune to the disease, especially through vaccination.
Thanks for reading and watching. Please stay safe and healthy in this time,
-Dr. Paul Thomas with Plum Health DPC
Single Largest Jump in Coronavirus Cases in a 24 Hour Period
Coronavirus Update: United States sees the single biggest increase in cases in a 24 hour period
Unfortunately, the United States has just witnessed the single largest increase in Coronavirus cases of any country in a 24 hour period. Over the last 24 hours, there have been 14,550 new cases reported in the United States according to this website.
Why is the Coronavirus Spreading so quickly in the United States?
It comes down to the concept of R⌀.
R⌀ is the average number of people that an infected person transmits the virus to.
If R⌀ is <1, the epidemic will burn out.
If R⌀ = 1, then epidemic will continue at a steady pace.
If R⌀ >1, the epidemic will increase exponentially.
Current estimates put R⌀ at about 2.5 to 2.9 (Peng PWH et al, 2/28). In plain English, this means that the average person with the Coronavirus will give the virus to 2.5 to 2.9 other people. This transmission rate is a bit higher than seasonal influenza. R⌀ is a reflection of both the virus and also human behavior. Interventions such as social distancing and improved hygiene will decrease R⌀.
Control of spread of COVID-19 in China proves that R⌀ is a modifiable number that can be reduced by effective public health interventions. The R⌀ on board the Diamond Princess cruise ship was 15 – illustrating that cramped quarters with inadequate hygiene will increase R⌀ (Rocklov 2/28).
The Coronavirus started with a single infected person, and it spread to roughly 2.5 to 2.9 other people. Once infected, those people passed the Coronavirus to another 2.5 to 2.9 people each. This is how a virus can exponentially spread. The Coronavirus spread has been hard to diminish because people have a relatively long incubation period or they have the virus and they don’t show symptoms of having the virus for a relatively long period of time, like 5 days to 10 days.
What should I be doing during the Coronavirus pandemic?
Definitely stay at home as much as possible. If you must go outside your home, practice social distancing and act as though you have the virus. Essential tasks done outside the home include buying groceries, making visits to the doctor, and picking up medications from the pharmacy.
How do I protect myself when I go outside?
First, avoid going outside unless you’re going for a walk or otherwise exercising in your neighborhood. If you must go outside, wear disposable latex gloves when you touch high-risk surfaces. For example, when you pump gas at the gas station, put on a pair of latex gloves during the credit card use, key pad entry, and handling the gas pump. Then, dispose of the gloves responsibly in a nearby trash can. Use hand sanitizer once you’re back in your car. Don’t touch your eyes, nose, or mouth after touching potentially contaminated surfaces. You can also use this routine of wearing latex gloves when grocery shopping or when handling a grocery cart.
Is it safe to get food delivered?
Yes, it’s safe to have food delivered and it’s safe to get take-out food. The best practice is to wash your hands after touching any packaging and to wash your hands again before eating. For instance, if you get your food in a brown paper bag, take your food out of the brown paper bag, recycle or discard the brown paper bag, and wash your hands before touching the food or individually wrapped food. Then, transfer the food to a plate or glass bowl and microwave the food for 30 seconds. This will kill any germs or bacteria in or on the food. Wash your hands again prior to eating.
What can you do to boost your immune system?
Many people want to know what they can do to boost their immune system to protect themselves from the Coronavirus. You can do the following to boost your immune system:
Sleep 7 to 9 hours each nigh
Eat nutritious and healthy foods
Drink plenty of fluids, mostly water
Exercise for 1 hour each day
Meditate to keep your stress levels low
When we’re stressed out, we tend to produce more cortisol, a steroid hormone that can weaken our immune system. That’s why it’s important to meditate, sleep well, and exercise.
What are good exercises during the Coronavirus quarantine?
You definitely want to exercise every day during the Coronavirus quarantine. Exercise will be good for your physical health, immune system, and emotional wellbeing. The best exercises will be to go outside of your house for a walk, jog, run, or bike ride. This is one of the few exceptions to the “stay at home” rule above. When you exercise, make sure that you’re keeping your distance from other people by at least 6 feet. You can exercise in your neighborhood or a nearby park. Avoid mall walking or any exercise where you’ll have to open a door/use a door handle for entry. That’s why we recommend folks avoid gyms and pools because there are just too many surfaces that could harbor the Coronavirus and potentially spread the infection. Therefore, exercise at home: lift weights, do floor exercises, do yoga or pilates. Fortunately, several health and fitness companies are giving free 30 day trials of home exercises - take advantage of these programs.
What can you do to slow down the Spread of Coronavirus?
Stay at home.
Act as though you have the virus and any interaction is a potential to spread the virus to a vulnerable person. People who are the most vulnerable are older adults or those with pre-existing medical conditions like lung diseases or cardiovascular diseases.
Do not visit nursing homes or elderly relatives, even if you feel well. You could be an asymptomatic carrier of the coronavirus and you could potentially endanger or kill the older adults that you visit.
Should you be sitting on a stockpile of extra medical supplies and equipment, please donate it to your nearest hospital or primary care physician office. If you have new and unused N95 masks or gloves, please donate them to these healthcare facilities.
Thanks for reading and watching, and have a wonderful day.
-Dr. Paul Thomas with Plum Health DPC
Detroit Doctor on AskASwimPro Show with Fares Ksebati
This week, I was invited on the AskASwimPro Show with Fares Ksebati. Fares is the CEO of MySwimPro, an App that helps swimmers improve their stroke, among other things. From their website:
MySwimPro is using technology to advance the sport of swimming and help swimmers all over the world achieve their goals in new and exciting ways. The platform is more than just an app, it's a community that keeps you accountable and pushes you to do your best.
In general, we had an informative discussion about the Coronavirus and its impact on our communities, specifically swimmers. Here’s what the MySwimPro team wrote about on their blog, found here:
In this episode of the #AskASwimPro Show, we interviewed Dr. Paul Thomas of Plum Health about the novel coronavirus, how to practice social distancing, the importance of “flattening the curve” and how swimmers can stay safe.
Dr. Thomas explained that many of us have had a coronavirus before, but that COVID-19 is more contagious. COVID-19 has a mortality rate of 3.5%, compared to the seasonal flu’s mortality rate of 0.1%, he says.
The virus spreads through coughing and inhaling someone else’s respiratory droplets. Due to this, Dr. Thomas explained that it isn’t wise to fly right now, since airplanes place you in close proximity to others.
He also noted that COVID-19 can live on surfaces for up to 3 days:
Stainless steel and plastic: 3 days
Cardboard and paper products: 24 hours
Copper: 4 hours
We go on to discuss social distancing:
Social distancing involves staying 6 feet away from others when you are outside, and avoiding contact with others while at home. You risk transmission any time you talk, shake hands or spend time around others. Dr. Thomas recommends that people avoid gathering with others and stay home in “self-quarantine,” noting that in cultures where it is common to kiss each other on the cheek or shake hands, COVID-19 can spread very quickly.
If you get COVID-19, you will be quarantined for at least 14 days, Dr. Thomas said. However, researchers have mentioned that you may be able to infect others for up to 20 days after showing symptoms.
We then discuss Flattening the Curve:
The healthcare system in the United States can only manage so many patients at one time, Dr. Thomas said. By practicing social distancing, we can “flatten the curve,” reducing the number of COVID-19 cases at a given time and keeping healthcare providers within their capacity. If we don’t do this, Dr. Thomas noted that the U.S. healthcare system will be unable to effectively care for patients.
We then talked about how you can stay safe during this Coronavirus Pandemic:
Dr. Thomas shared tips to stay safe and healthy:
Wash your hands: Before you prepare food, after going to the bathroom and before touching your face.
If you have a cough or a low grade fever (99 or 100 degrees Fahrenheit): Stay home, drink lots of fluids, take Tylenol and get some rest. You likely are not sick enough to benefit from a doctor’s treatment. Save the hospital beds — and the healthcare providers’ time — for those who are sickest!
If you have severe symptoms, such as a high fever and trouble breathing: Go to the hospital.
Thanks for reading and watching,
-Dr. Paul Thomas with Plum Health DPC